

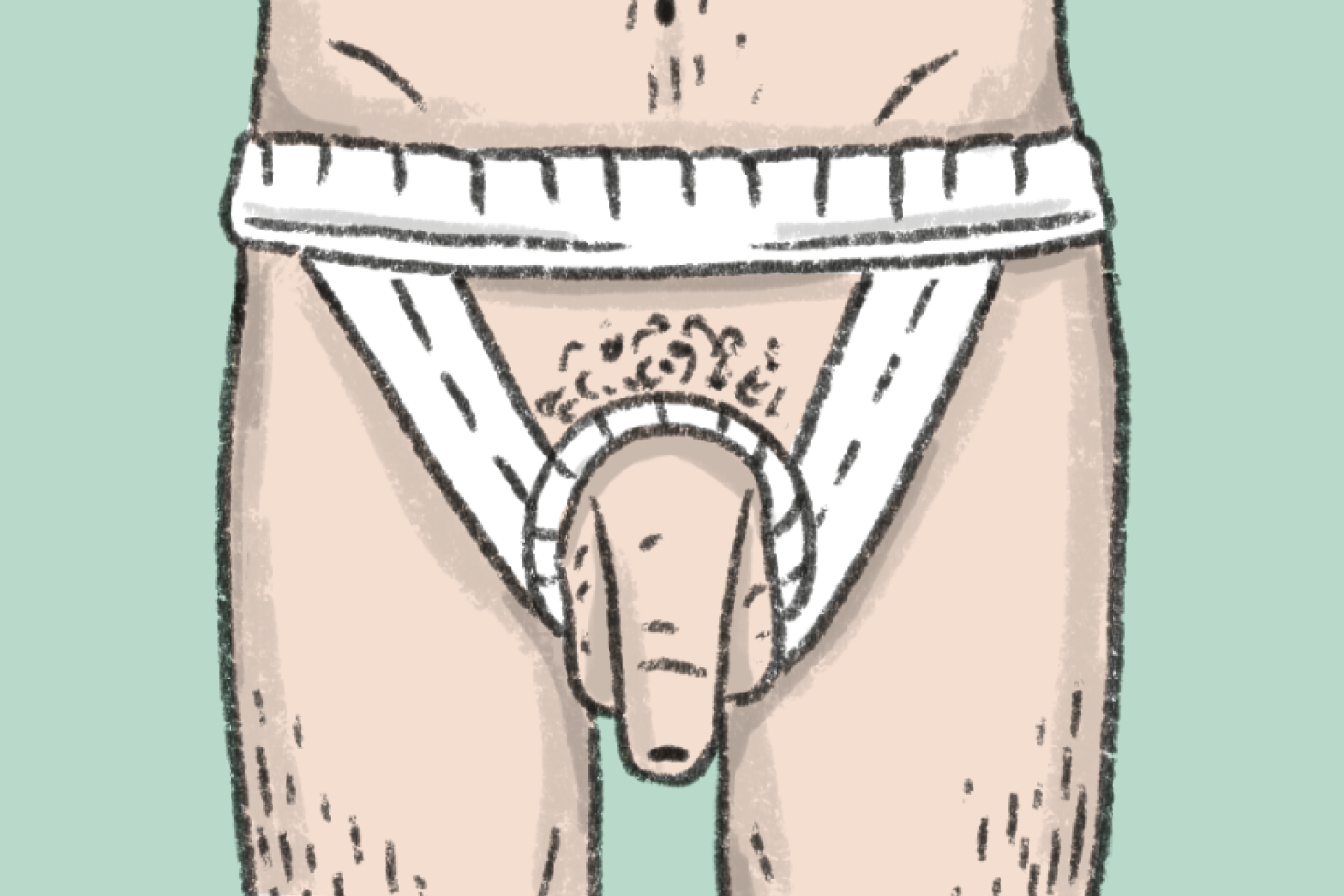
Heated underpants, a contraceptive ring: Alongside the search for chemical molecules, hormonal or otherwise, male contraception could involve another – thermal – approach. In principle, the blocking effects on spermatogenesis of increasing the temperature of testicles by a few degrees have been known for decades. In practice, more and more men resort to devices – often homemade – which are designed to move testicles up to the entrance of the inguinal canal for contraception. To date, there has been no validation by the health authorities, but this could change over the next few years.
Although the story began in India in the 1930s, with Swiss physician Martha Voegeli's experiments showing a drop in male fertility thanks to daily hot baths, it was picked up in France, originally in Toulouse. In the 1980s, andrologist Roger Mieusset (andrology is the medical specialty that explores male genitalia) and reproductive biologist Louis Bujan were part of a male group examining questions of paternity and male contraception. "In that group, a farmer who spent a lot of time on his tractor told us he could feel his testicles moving upwards," Bujan recalled. That is how Mieusset, who was already working on the subject of hyperthermia and its negative effects on spermatogenesis, came up with the original idea of an adapted undergarment. In 1987, he published the method. In 1994, the two doctors from Toulouse reported the results of a preliminary study in the International Journal of Andrology. It involved nine couples and over 150 cycles, indicating that the underpants were an effective, well-tolerated and reversible method of contraception. To achieve a drastic drop in sperm counts (below the threshold of 1 million/ml sperm), they must be worn for at least 15 hours a day. In 1991, Egyptian researcher Ahmed Shafik published comparable results in some 30 men who underwent (reversible) testicular suspension surgery.
'Many requests'
In the years that followed, there was little progress in the research due to a lack of interest on the part of other teams and industrial partners to replicate the clinical studies and carry them out on a larger scale. The concept was never taken very seriously. "I think it is a pity that a manufacturer did not develop the product after Dr. Mieusset had patented the device. We would have had standardization, responding to a growing demand," said Professor Bujan. This attitude was echoed by François Isus, general practitioner and andrologist, who succeeded Mieusset in the Department of Reproductive Medicine and Biology at Toulouse University Hospital. In France, vasectomy sterilizations have increased tenfold over the last decade, with more than 21,000 performed in 2021. "I get a lot of requests for thermal contraception, and limit myself to 5-10 consultations a week," said Isus. "I can't prescribe it, since it's not recognized, but I give information, examine these men to check for the absence of counter-indications, and run a spermogram." What comes next? Those who wish to do so can, under their own responsibility, make their own suitable underwear or buy a contraceptive ring (currently on sale as a decorative item). "A follow-up spermogram [a test for male fertility] would be necessary every three months, but the majority have no follow-up," said Isus, who is considering a new clinical study protocol.
You have 35% of this article left to read. The rest is for subscribers only.
