



Hit tumors hard and fast. This could be the new method for administering ionizing radiation, known as FLASH radiotherapy. This bold, innovative project was announced by the Institut Curie on World Cancer Day, Tuesday, February 4. The project involves the construction of a high-energy electron beam irradiator at the Orsay Hospital in the Paris region, due to be operational in 2026.
As its name suggests, FLASH radiotherapy involves exposing tumors to extremely short radiation durations (1,000 to 10,000 times shorter than conventional radiotherapy), but with rays 10 to 15 times more intense. The aim is to target tumors with a bad prognosis.


This strategy has not yet been evaluated with patients. Human trials are not scheduled to begin until 2028. However, major cancer treatment centers are already banking on this approach, to the point of investing in major equipment. The cost of the Institut Curie project, including preclinical studies, comes to €37 million, financed by the "Avenir France 2030" future investment plan (€35 million) and the Paris region (€2 million).
To justify such an investment, significant therapeutic benefits are expected. Its promises are threefold. The first is to target deeply located tumors (up to 20 or 30 centimeters beneath the skin) or close to vital organs – brain, lung and pancreas tumors, for example – but also tumors affecting children. The second challenge is to limit the after-effects of radiation. The third promise is to reduce the number and duration of radiotherapy sessions, thereby reducing the associated fatigue and transport costs.
"This is a real paradigm shift, with the ambition of curing more patients with bad-prognosis cancers," said Gilles Créhange, head of the Radiation Oncology Department at the Institut Curie, who is coordinating the project. "By reducing toxicity, FLASH radiotherapy should make it possible to increase irradiation doses without causing damage."
More than 10 articles on this new technique are published every month. FLASH radiotherapy brings together physicists, biologists, engineers and doctors from all over the world at annual conventions.
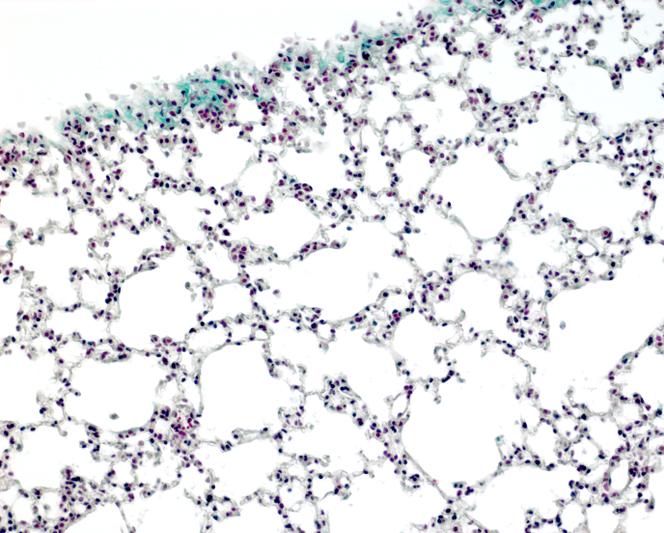
"This project was born in a laboratory at the Institut Curie in Orsay in the early 2000s," explained Alain Puisieux, chairman of the Institut Curie Board of Directors. A researcher there, Vincent Favaudon, made an unexpected observation. Fractioned doses of irradiation created the same damage as conventional irradiation on tumor cells in culture but spared healthy cells. In 2014, he published the first demonstration of this "FLASH effect" in mice. In the rodent, this mode of irradiation inhibits the growth of lung tumors with the same efficiency as conventional irradiation, but without triggering fibrosis in the lungs (an excess of fibrous tissue, leading to respiratory discomfort) or damaging the skin.
In 2020, FLASH radiotherapy proved effective in treating ovarian cancers in mice, while reducing gastrointestinal toxicity and associated mortality. In the same year, the team led by Charles Fouillade, radiobiologist and researcher at the Institut Curie, explored the mechanisms by which FLASH irradiation works on normal mouse lungs. "FLASH radiotherapy reduces DNA damage in normal lung cells," he said. "It also preserves the stem cells of this lung epithelium, hence its regenerative capacity."
But how to explain the preferential damage to cancerous tissue? "This is not entirely clear," said Fouillade. "The role of oxygen, a powerful radiosensitizer, has been suspected, but the hypothesis has not been confirmed."
In 2017 and 2023 respectively, Swiss and American teams studied how brain irradiation affected – or not – the cognitive faculties of normal mice. Verdict: With FLASH radiotherapy, the learning capacities and memory of rodents are preserved, but not with conventional radiotherapy. The protective effect, in FLASH mode, seems to be linked to a reduction in neuroinflammation and the maintenance of synapse plasticity, areas of communication between neurons.
However, a warning signal emerged in 2022. In three of seven cats with spontaneous muzzle cancers, a single dose of FLASH radiotherapy caused maxillary bone necrosis nine to 15 months after treatment. This late toxicity calls for "caution," according to Marie-Catherine Vozenin, from the University of Lausanne in Switzerland, who initiated the study.
This is why, once the accelerator is built, a great deal of work remains to be done before the first clinical trials can be initiated. In partnership with the French Atomic Energy Commission (CEA), a series of milestones have yet to be achieved. Physicists will have to develop dosimetry and imaging equipment, as well as radiation protection protocols. The Curie project benefits from a bunker that has already been built, surrounding one of the three unused proton therapy treatment rooms at the Orsay hospital. This protection is indispensable.
FLASH RADIOTHERAPY, AN INNOVATIVE PROJECT FROM INSTITUT CURIE
Source: Institut Curie
Infographic: Le Monde, Victoria Denys, Florence Rosier
The radiobiologists will have to dissect the biological impact of the FLASH effect on animal models while defining optimal treatment doses. Because everything will have to be reworked. Until now, most of the work on FLASH radiotherapy has used low-energy electron accelerators, "with which we can only treat superficial tumors," said Créhange.
In Villejuif, on the southern Paris outskirts 25 kilometers north of Orsay, the Gustave-Roussy Institute, Europe's leading cancer center, is also banking on FLASH radiotherapy. As a first step, it will assess the safety of this approach, but using a low-energy electron source. "By the end of 2025, we hope to launch a first clinical trial on a dozen patients with skin cancers," said Eric Deutsch, head of the radiotherapy department at Gustave-Roussy.
The institute is also developing its own project for a high-energy electron accelerator. The project, selected by an international jury at the end of 2023, will be financed to the tune of €38 million by the France 2030 plan. Theryq, the manufacturer entrusted with this project, will also produce the accelerator for Lausanne University Hospital, which is exploring this approach.
On the other side of the Atlantic, the University of Pennsylvania is equally interested in FLASH radiotherapy, but with a different source of radiation: Protons. In 2023, the university published the results of its first-ever FLASH proton therapy clinical trial involving 10 patients with bone metastases from various cancers. This preliminary work demonstrated the feasibility of the treatment.
Translation of an original article published in French on lemonde.fr; the publisher may only be liable for the French version.
