

Authored by Teri Ward via The Epoch Times (emphasis ours),
Peripheral neuropathy (PN) is a severe and complex neurological disorder affecting 20 million to 30 million people in the United States.
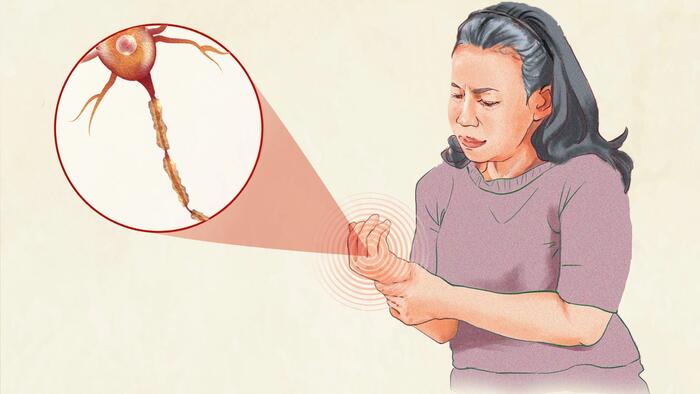
PN damages nerves outside the brain and spinal cord, primarily in the feet and hands. Symptoms such as numbness, tingling, burning pain, and muscle weakness can drastically reduce quality of life, making even simple tasks challenging.
Identifying and treating the root cause of PN is vital to prevent further nerve damage and preserve mobility. If left unaddressed, PN can lead to severe complications, including the risk of limb amputation.
Recognizing the symptoms of PN is necessary for early diagnosis and treatment to prevent irreversible damage. Common early warning signs include numbness that may feel like “walking on pillows” and pain or burning sensations in the feet or hands.
PN can manifest differently depending on the cause and the type of nerves affected. Symptoms vary widely; some individuals experience severe pain, while others might have numbness with little discomfort. The onset can be gradual, as seen in diabetic peripheral neuropathy (DPN), or sudden, as in neuropathy from toxic exposure or Guillain-Barré syndrome.
Typically, PN follows a “stocking and glove” pattern, starting at the feet and progressing upward, eventually affecting the hands. This pattern occurs because the longest nerves are most susceptible to damage due to issues like reduced blood flow and metabolic disturbances.
Peripheral nerves consist of sensory, motor, and autonomic nerves, with symptoms varying based on which type is affected. The severity and progression of symptoms also depend on whether the nerves are myelinated (with a protective sheath) or unmyelinated. Damage can be axonal or demyelinating, affecting the nerve fibers or the myelin sheath, respectively.
These nerves transmit sensations like touch, temperature, and pain. Many sensory nerves, especially pain-sensing fibers, are unmyelinated and may be affected more gradually. Damage can cause:
These nerves control muscle movement. Most motor nerves are myelinated, allowing faster signal conduction and potentially quicker symptom onset when damaged. When affected, symptoms may include:
These nerves regulate involuntary functions and may be myelinated or unmyelinated. Symptoms include:
PN is not a single condition but rather a group of related disorders that can have various causes and symptoms. PN occurs when the peripheral nerves, which connect the brain and spinal cord to the rest of the body, are damaged. This damage can occur through various metabolic and cellular pathways, affecting the nerves in different ways but ultimately leading to disruptions in nerve function. The development is often complex and likely involves multiple contributing factors.
The following list of mechanisms and causes is not exhaustive, and ongoing research continues to uncover new insights, but some of the leading causes include the following:
There are many different types of PN. It is classified in numerous ways, including by the nerves affected, underlying causes, and symptom characteristics. Some of the ways PN can be classified include the following:
PN risk is influenced by various factors, some of which cannot be changed (unmodifiable) and others that can potentially be controlled through lifestyle choices (modifiable). Factors that increase the risk of developing PN include the following:
Early diagnosis, identifying the cause, and ruling out other conditions is key to effective treatment. Diagnosing PN takes a step-wise approach.
In the first step, symptoms are assessed, and a detailed history is taken to obtain information about alcohol use, family history of neuropathy, recent illnesses or vaccinations, and use of neurotoxic medications such as gout medications, antivirals, and chemotherapy. Additionally, information about blood transfusions, sexual history, and intravenous drug use is gathered to assess HIV and hepatitis C as potential causes.
Clinical and neurological examinations follow, evaluating muscle strength, reflexes, and sensitivity to temperature, light touch, position, and vibration. The practitioner will consider the onset and progression of PN, whether symptoms are symmetrical or asymmetrical, their location, and the nerves involved, providing clues to the underlying causes and type of neuropathy.
Urgent referral to a neurologist is warranted for individuals experiencing sudden, severe, or worsening symptoms to ensure prompt treatment. This is particularly critical for those showing nerve damage in multiple areas, unusual patterns, or having only motor or autonomic symptoms without sensory changes.
Absent indications of referral necessity, this initial assessment may lead to a clinical diagnosis of PN. However, even in diabetics, additional testing is essential to eliminate other potential coexisting causes.
Laboratory tests help identify contributing factors and rule out other conditions. Depending on the individual’s clinical presentation and diagnostic findings, blood tests may include:
Some of these tests may be ordered by the primary care practitioner or a neurologist following referral.
If initial tests are inconclusive, symptoms are complex, or other health conditions are present, further testing or a neurologist referral may be necessary. A specialist can then conduct advanced tests to provide valuable insights into the extent and nature of nerve damage. These additional assessments may include:
Other less common, newer, or not widely available tests include VibraTip, corneal confocal microscopy, laser-evoked potentials, and quantitative sensory testing.
While peripheral neuropathy is often a complication of other conditions, it can lead to its own set of complications due to nerve damage. These include:
While these complications can be serious, there are steps that patients and their families can take to prevent or manage some of them effectively and improve quality of life. Here are some practical strategies:
Treating PN can be complex due to its many underlying causes and symptoms. The primary goal is to address the identified cause, such as managing blood glucose in diabetics or correcting vitamin deficiencies. In about 20 percent of cases, no cause is identified. However, symptoms can still be treated to improve quality of life, according to studies in Norway and the Netherlands, as mentioned in a 2020 paper in Neurological Research and Practice.
Traditional painkillers are typically ineffective for nerve pain, so other medications are generally utilized. Unfortunately, these medications do not work for everyone; they do not address the underlying cause of PN and often come with significant side effects.
Despite limited effectiveness and significant safety concerns, gabapentin is widely prescribed as a first-tier treatment for neuropathic pain. Some researchers recommend reconsidering its use. A Cochrane Review found that gabapentin provided over 50 percent pain relief to about 38 percent of people with painful DPN.
Safety concerns arise when gabapentin is taken with drugs like benzodiazepines and opioids. In a study of accidental mixed-drug deaths involving opioids, gabapentin was present in about 25 percent of cases. Adverse effects include daytime sleepiness, weight gain, edema, and dizziness, with additional concerns about cognitive impairment, dementia risk, addiction, abuse, misuse, and illegal distribution.
Another option is pregabalin. However, research shows that for the majority of people with painful DPN, pregabalin provides little relief. At a dosage of 300 milligrams, only one in 22 people experienced a reduction in pain of 50 percent or more.
Antidepressants, such as tricyclic antidepressants (e.g., amitriptyline, nortriptyline) and serotonin-norepinephrine reuptake inhibitors (SNRIs) (e.g., duloxetine), are effective in treating neuropathic pain. Duloxetine has been shown to provide better pain relief than pregabalin. These medications work by increasing levels of norepinephrine and serotonin in the nervous system, which helps reduce pain signals. Be sure to discuss the potential side effects with your prescribing practitioner.
Controlled-release oxycodone has been found to be an effective treatment in painful DPN with significantly improved quality of life. Tramadol, tapentadol, and other opioids may also be effective and are sometimes prescribed for severe neurologic pain. However, they should be used cautiously due to the associated high risk of addiction, misuse, illegal distribution, and when used with coexisting severe psychiatric conditions.
These treatments are used for severe neuropathies caused by inflammation or immune attacks on nerves, like chronic inflammatory demyelinating polyradiculoneuropathy (CIDP). Steroids reduce inflammation. Plasma exchange (PE) removes harmful antibodies from plasma and replaces it with a substitute solution. Intravenous immune globulin (IVIG), made from pooled antibodies from healthy donors, helps regulate the immune system.
As for topical medication, lidocaine patches or capsaicin cream may provide localized relief with few systemic side effects.
Other potentially effective treatments include surgery for cases of nerve compression, transcutaneous electrical nerve stimulation (TENS), spinal cord stimulation (SCS), physical and occupational therapy, acupuncture, and low-level laser therapy.
Studies show that combining traditional Chinese medicine (TCM) with Western medicine can improve effectiveness and nerve function. Emerging therapies such as ARA 290, a peptide, are also being explored for potential benefits in managing PN associated with sarcoidosis.
Peripheral neuropathy can significantly affect a person’s daily life, affecting mood, sleep, and overall quality of life. Chronic pain, numbness, and other symptoms associated with PN can lead to sleep disturbances, which in turn can exacerbate the perception of pain, creating a vicious cycle. Additionally, the financial burden of associated direct and indirect costs can create stress that further degrades quality of life.
While PN symptoms can influence mental state, mindset also plays a significant role in how individuals experience and manage their condition. A large study on various pain conditions found that certain thought patterns, such as thinking the worst about pain, fearing pain, and being overly aware of pain, are strongly linked to negative emotions, anxiety, depression, higher pain intensity, and greater interference with daily activities.
This research underscores the importance of addressing mindset in PN management. A positive mindset can be a powerful tool in coping with PN and potentially improving outcomes. Here are key aspects of how mindset influences PN:
While many people use natural and herbal remedies, scientific evidence supporting their effectiveness is often limited. What works for one person may not work for another. Natural products can cause adverse reactions, interact with medications, or be contraindicated with certain medical conditions. Consult your health care provider or pharmacist for personalized advice.
Natural approaches to peripheral neuropathy can complement conventional treatment effectively. The first step is to eliminate or minimize the causative agent. Before starting any necessary chemotherapy, optimizing nutritional status may help prevent PN or lessen its severity. Since nerves regenerate slowly and the body does not produce new nerves, patience is essential, especially with natural approaches, as damage can become irreversible over time. Below are some natural approaches backed by peer-reviewed research.
Research demonstrates that aerobic exercise can improve symptoms of PN, whether performed alone or in combination with resistance or balance training. A minimum of three weekly sessions of activities such as walking, cycling, or swimming is recommended. Simple exercises, including leg stretches and balance movements, can also enhance nerve function and reduce pain. Regular exercise can potentially delay progression, improve symptoms, and, in some cases, even reverse symptoms. It can also enhance blood flow, reduce cellular damage, and stimulate nerve regeneration.
A gluten-free diet (GFD) can effectively reduce neuropathic symptoms and improve quality of life in those with gluten neuropathy, a type of peripheral neuropathy linked to gluten sensitivity. A small study found that those who strictly followed a GFD experienced better pain management and overall health compared to those who continued eating gluten. Gluten is incompletely digested and can cause inflammation by increasing intestinal permeability, even in individuals without gluten sensitivity.
Omega-3 fatty acids help reduce inflammation, regulate blood pressure, glucose tolerance, and nervous system development and function.
Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are two important omega-3 fatty acids primarily found in fatty fish. EPA is known for its anti-inflammatory properties, while DHA is crucial for brain health. A small pilot study found that supplementing with 1,000 milligrams of DHA and 200 milligrams of EPA for three months helped reduce pain in DPN.
One study found that gamma-linolenic acid (GLA) was as effective as alpha-lipoic acid (ALA) in reducing pain, although ALA may work more quickly in those with better kidney function. It is found in borage, evening primrose, and blackcurrant seed oils.
Research has shown that supplementing with certain vitamins, minerals, and other nutrients can improve symptoms and quality of life for those with peripheral neuropathy. These beneficial nutrients include:
Individual supplementation or a professional formulation may be necessary to achieve therapeutic doses. While most B vitamins are safe in high doses, excess vitamin B6 can damage nerves and induce or worsen neuropathy.
Preventing peripheral neuropathy involves maintaining good metabolic, vascular, and nerve health. Just as the risk of peripheral neuropathy increases with each component of metabolic syndrome, the protective benefits increase with each healthy diet and lifestyle change. Here are some key strategies:
