A new study found more than 1 million U.S. deaths a year—including those in young people and working-age adults—would have been averted if the United States had mortality rates similar to other wealthy nations.
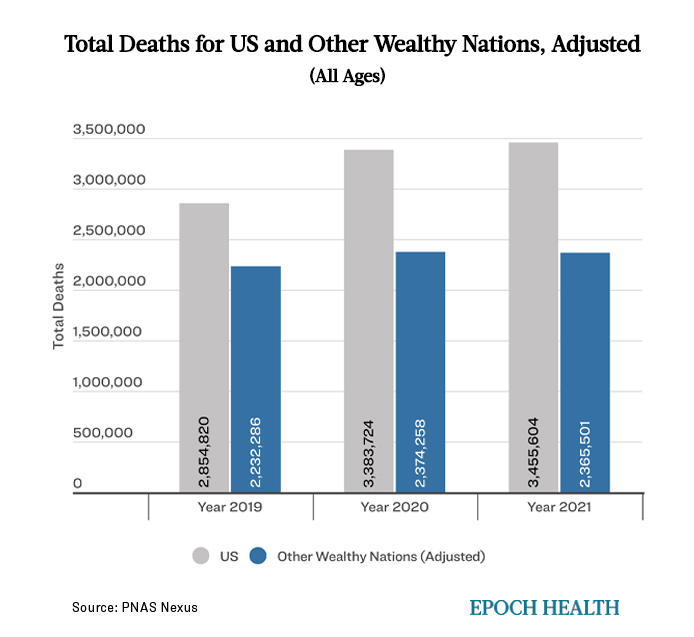
Published in the journal PNAS Nexus, researchers assessed how many U.S. deaths would have been avoided each year from 1933 through 2021 if U.S. age-specific mortality rates had equaled the average of 21 comparable wealthy nations.
The analysis includes Australia, Austria, Belgium, Canada, Denmark, Finland, France, Germany, Iceland, Ireland, Italy, Japan, Luxembourg, the Netherlands, New Zealand, Norway, Portugal, Spain, Sweden, Switzerland, and the United Kingdom.
Using mortality data from the Human Mortality Database and the Centers for Disease Control and Prevention, results showed the U.S. had mortality rates lower than peer countries in the 1930s-1950s, similar mortality rates in the 1960s and 1970s, and experienced a steady rise in the number of “missing Americans” in the 1980s.
“Missing Americans” refers to U.S. excess deaths—people who would still be alive today if the United States had mortality rates equal to other peer nations.
According to the study, there were 622,534 excess deaths in 2019. Numbers surged higher during the COVID-19 pandemic reaching 1,009,467 excess deaths in 2020, and 1,090,103 in 2021.
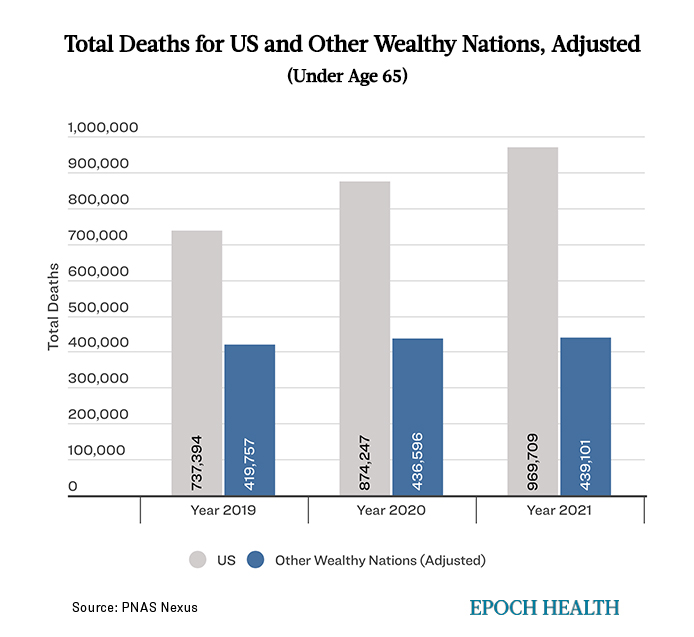
Excess mortality was exceptionally high in people under age 65, with nearly 50 percent of excess deaths occurring in 2020 and 2021, despite data showing young people were least likely to die of COVID-19.
“The number of Missing Americans in recent years is unprecedented in modern times,” the study’s lead author Dr. Jacob Bor, associate professor of global health and epidemiology at Boston University School of Public Health, said in a press release.
Dr. Bor is particularly concerned about excess mortality among working-age adults: “Think of people you know who have passed away before reaching age 65. Statistically, half of them would still be alive if the U.S. had the mortality rates of our peers,” he said. “The U.S. is experiencing a crisis of early death that is unique among wealthy nations.”
According to the study, excess U.S. mortality is linked to several factors, including drug overdoses, firearm injuries, car accidents, cardiometabolic disorders, and smoking.
During the 2020-21 COVID-19 pandemic, increased mortality could not solely be attributed to a novel pathogen, as other wealthy nations were also exposed. Instead, the researchers attributed the rise in mortality to socioeconomic inequality, a limited safety net, low vaccine uptake, and politics, with “residential segregation, limited ability to work from home, distrust of the medical establishment, decreased access to health care, and a higher prevalence of comorbid conditions” adding to the excess risk in low-income and minority populations.
Although two-thirds of excess deaths occurred in white Americans, black and Native Americans were disproportionately affected—as were individuals with low income and education levels.
“We waste hundreds of billions each year on health insurers’ profits and paperwork, while tens of millions can’t afford medical care, healthy food, or a decent place to live,” co-author Dr. Steffie Woolhandler, professor at the School of Urban Public Health at Hunter College in New York, said in a press release. “Americans die younger than their counterparts elsewhere because when corporate profits conflict with health, our politicians side with the corporations.”
Dr. Bor is not optimistic mortality trends will reverse as COVID-19 wanes because the United States was already experiencing more than 600,000 excess deaths annually before the pandemic began, and there have been no substantial policy changes to alter this trajectory.
“While COVID-19 brought new attention to public health, the backlash unleashed during the pandemic has undermined trust in government and support for expansive policies to improve population health,” said Dr. Bor. “This could be the most harmful long-term impact of the pandemic because expansion of public policy to support health is exactly how our peer countries have attained higher life expectancy and better health outcomes.”
Considering future lives lost due to premature death, the authors estimate that in 2021 alone, excess U.S. mortality translated to 26.4 million years of life lost compared to the mortality rates of other wealthy nations.
What topics would you like to read about? Please let us know at health@epochtimes.nyc