Strokes, or brain attacks, are a leading cause of death in America (pdf). In 2020, stroke caused 1 out of 21 deaths (pdf) in the United States. Luckily, many who survive a stroke can recover with minimal complications. Rehabilitation and lifestyle changes can improve recovery and minimize the risk of recurrence.
A stroke is a medical emergency caused by a loss of oxygen to the brain. Within minutes, brain cells die, which can result in lifelong complications or even death.
Recognizing the symptoms or signs of a stroke quickly will improve the chances of successful recovery.
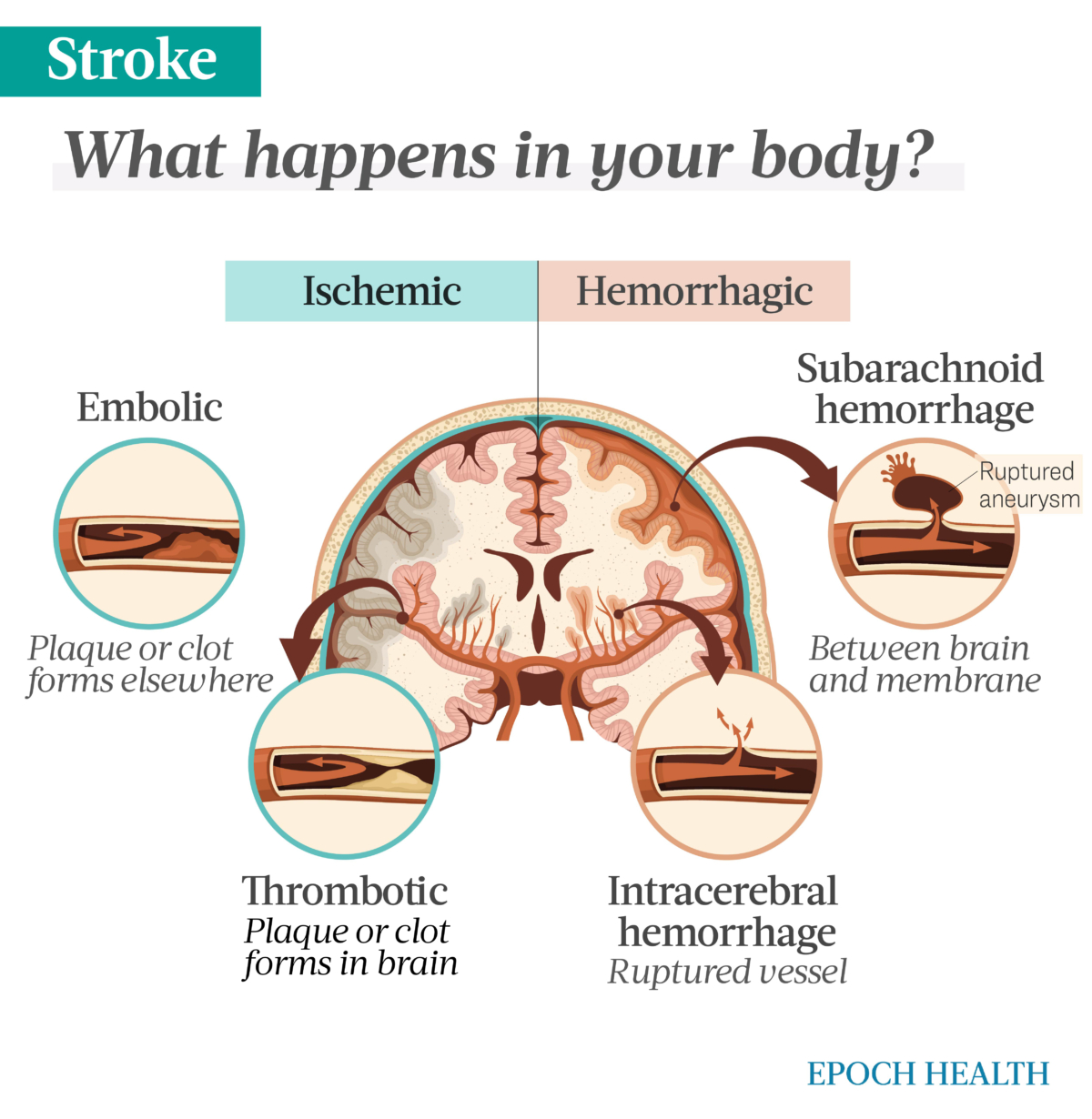
There are two common types of stroke, each with two subtypes. What causes the interruption of oxygen and blood flow to the brain is what differentiates them. The following are the two main types of stroke and their subtypes:
Quickly recognizing the signs or symptoms of stroke can significantly improve the stroke patient’s outcomes. A simple acronym to help remember the signs and symptoms of stroke is F.A.S.T.:
Less frequent symptoms can include:
A stroke’s cause depends on its type. Ischemic strokes are caused by blockage, while hemorrhagic strokes are caused by a leaking or burst blood vessel or ruptured aneurysm.
An ischemic stroke is the most common type, with approximately 87 percent of all strokes being ischemic. Ischemic strokes are caused by blockage.
An artery can become blocked in multiple ways. A buildup of fatty deposits (plaque) or a blood clot can block a vessel.
A transient ischemic attack (TIA) is a temporary disruption of blood flow to the brain. The interruption resolves within minutes and usually does not result in permanent complications. These are sometimes referred to as ministrokes.
Leaking or burst blood vessels can cause a hemorrhagic stroke. Several factors can contribute to this:
When blood leaks or bursts from the blood vessel, it puts pressure on brain tissue. This pressure damages brain cells, leading to hemorrhagic stroke.
A few mechanisms are behind the primary causes of stroke: blockage (ischemic) or a leaky or burst vessel (hemorrhagic). The mechanisms are detailed below.
The buildup of plaque in the arteries can become hard, causing atherosclerosis. As hardening plaque collects in the vessel, passage through the vessels narrows, limiting blood flow.
The plaque building up on the artery wall can break. Platelets in the blood can then stick to the damaged area of the plaque and form a clot. The clot can partially or fully block the artery. According to the National Institute on Neurological Disorders and Stroke, this is the most common way arteries become blocked. Inflammation may also cause artery blockage by promoting plaque accumulation.
Ischemic strokes are divided into two types:
Thrombotic: Thrombotic strokes occur when plaque buildup causes blood proteins to accumulate into a complete blockage, called a thrombus. The plaque or clot can travel to the brain from elsewhere in the body, but the blockage occurs in the brain.
Embolic: Embolic strokes result from a clot that has developed elsewhere in the body that disrupts blood flow to the brain. An artery may become blocked by a traveling blood clot from the left side of the heart or the carotid arteries or by debris (for example, from an infected heart valve). Untreated atrial fibrillation, a common arrhythmia of the heart, is a risk factor for emboli to the brain.
A hemorrhagic stroke is when a blood vessel in the brain leaks or bursts. As pressure builds within the brain from the bleeding, cells become damaged. As their access to oxygen further declines, they begin to die.
Hemorrhagic strokes account for about 13 percent of all strokes. This type is further divided into two categories:
Intracerebral: An intracerebral hemorrhage results from bleeding into the main tissue of the brain. This type of bleeding may also be called parenchymal hemorrhage.
An intracerebral hemorrhage occurs swiftly and without warning. These strokes can be severe and lead to coma or death.
Subarachnoid: With subarachnoid hemorrhaging, the bleeding happens in the space between the brain and its surrounding membrane. This space is called the subarachnoid space.
An aneurysm can cause bleeding in this space. An aneurysm is a bulge in a weakened part of the blood vessel wall.
Many factors can put a person at risk for stroke. Some factors can be controlled by lifestyle, while others cannot. The following factors increase a person’s risk for stroke:
Some studies find that women may experience more severe strokes and are more likely to die from them, as they tend to have strokes at an older age. They also have unique risk factors, such as pregnancy, childbirth, and menopause. Contributing risk factors during pregnancy are:
The risk of stroke is higher in adults over 55 and increases with age. Older people have a higher prevalence of ischemic stroke, which may be due to higher cholesterol levels, diabetes, or atherosclerosis.
According to the National Institute on Neurological Disorders and Stroke, children are at the highest risk of stroke during the perinatal stage of pregnancy. This period is before birth and a couple of weeks after. Children are often vulnerable at this stage due to congenital heart problems or head trauma. Generally, black children are at a higher risk, typically because sickle cell anemia (a sickle cell disease) is a high stroke risk.
The symptoms of stroke in children are similar to those in adults. Children may have a headache and paralysis or weakness on one side of the body. Other symptoms may include seizures, difficulty breathing, and loss of consciousness.
For children, the outcomes are worse than those of adults if the stroke occurs when the child is younger than 1 year old and if they lose consciousness during the stroke, regardless of age. However, children who have a stroke generally fare better than adults in rehabilitation due to the brain’s ability to adapt and rewire.
Socioeconomic factors have also been shown to affect the risk of stroke. Strokes are more common among those with a lower income. One reason may be the links between smoking and obesity, which occur more often in lower-income populations. Another explanation may be the population’s more limited access to health care.
People with other conditions, including the following, are also more at risk:
While there are several risk factors that a person can’t modify, many more can be modified, including:
Symptoms alone can’t determine if you have had a stroke. Once you arrive at the hospital, a medical team will conduct tests to determine if you had a stroke, TIA, or other medical event.
Health care providers will initially do a neurological exam with a questionnaire and physical tests. Providers will then use a scale to assess stroke severity. Typically, this is the standardized NIH Stroke Scale.
Other scales, such as Glasgow Coma Scale and the Modified Rankin Scale, may also be used. These types of scales help to measure the stroke’s resulting disabilities.
Health care providers may use other tests, such as:
There are many possible complications of stroke. The severity and duration depend on where the stroke occurred and how long the brain was without oxygen.
The more common complications of stroke are:
Each area of the brain is responsible for different bodily functions. Because of this, the stroke’s origin determines what complications a person will have. It also determines the severity and duration of those complications, which may be permanent or temporary.
The following are other complications that may be less common:
Treatments for stroke depend on its type. For ischemic strokes, treatment includes medications that will break up clots, procedures to remove clots, and restoration of blood flow to the brain. Treatments for hemorrhagic strokes involve procedures to stop a leaking blood vessel or repair a burst vessel, such as surgical clipping and coiling of the vessel.
Drug therapy is the most common treatment for early ischemic stroke. Clot-busting medications can be very effective when treating ischemic stroke. The caveat is that they have to be given soon after the signs or symptoms of a stroke begin.
For this reason, it is essential to note the time a stroke occurs. Medications that break up clots—thrombolytic drugs—need to be given within three hours of the onset of symptoms to be effective and are given intravenously. These types of drugs can significantly improve a person’s chance for a faster recovery.
Restoring blood flow to the brain as quickly as possible during an ischemic stroke can mitigate damage caused by the lack of oxygen to the brain. When oxygen returns, cells stop dying, and tissue that wasn’t damaged remains unharmed.
Medications are not the only way to restore blood flow to the brain when a vessel is blocked. A physician may opt to remove the clot with a stent retriever. A catheter is run through the blood vessel to the clot and retrieves it. This procedure may be used in conjunction with medication.
Before a vessel can be fixed or a leak can be stopped, the troubled vessel has to be located. Once a physician locates the bleeding, he or she performs one of two procedures: clipping or coiling.
Clipping is one way to treat brain aneurysms before they burst. These weak areas of vessels can expand like a balloon that may eventually burst. In this case, the aneurysm will have sprung a leak.
A neurosurgeon will then perform the clipping procedure. A clamp is put on the neck of the aneurysm to prevent it from bursting. Patients must be closely monitored after this procedure.
The other option is a coiling technique called endovascular embolization. Endovascular embolization is used for more high-risk cerebral aneurysms. A coil is placed in the aneurysm, triggering an immune response from the body. This results in the formation of clots on the wall of the aneurysm, which restores some strength to those weakened walls.
Should there be a case where neither procedure repairs the aneurysm, it may be necessary to occlude (close) the vessel. This stops blood flow to the vessel before it reaches the area of the aneurysm. No longer having blood flow to the aneurysm removes the risk of leak or rupture.
While these are ways to address the stroke itself, they do not address the consequences of a stroke. Recovery from the physical consequences of a stroke calls for rehabilitation.
Rehabilitation is essential to recovering from a stroke’s physical and mental complications. Rehabilitation can include:
Rehabilitation will begin as soon as possible. During the first few days of rehabilitation, sessions can be as often as hourly. While the patient remains in the hospital, sessions can be up to six times daily. When out of the hospital, rehabilitation can occur in an inpatient rehabilitation facility, where a patient will remain until rehabilitation is complete.
Some newer treatments are the Neurolutions Upper Extremity Rehabilitation System and the MicroTransponder Vivistim Paired VNS (vagus nerve stimulation) System.
The Neurolutions Upper Extremity Rehabilitation System is available to people 18 years and older with a disability of the upper arm due to a stroke. This system requires the person to wear a hand brace. The hand brace works with a table and electrodes that record brain activity and tell the brace to move the hand.
The MicroTransponder Vivistim Paired VNS System is used along with stroke rehabilitation for persons with upper extremity impairment due to chronic ischemic stroke. This system stimulates the vagus nerve in an effort to improve the motor function of the upper extremities.
A person’s outlook on life and how they perceive their rehabilitation can help prevent a stroke and help when rehabilitating from one.
Studies have shown that optimistic people have a lower risk of death from stroke. Optimistic people also tend to have better coping abilities than pessimistic people.
Negative emotions create a physical stress response and release hormones that can increase the heart rate and blood pressure, risk factors for stroke. People with a negative outlook may end up coping by self-medicating and may use other substances that can also increase the risk factor of stroke.
Mental illness can increase the prevalence of stroke risk factors as well. People with mental illness are more likely to smoke, be obese, and have high blood pressure and diabetes.
Adults with mental illness are also more likely to have cardiovascular disease, increasing stroke risk. This risk can increase over time.
There are many complementary and alternative treatments and prevention methods for stroke—from newer techniques to the more traditional approaches in holistic practices.
Behavioral changes can minimize many stroke risk factors, yet motivating people to make those changes can be challenging. Fortunately, the emergence of technologies such as digital phenotyping, social network analysis, machine learning, and gamification may be able to facilitate existing behavioral interventions. Encouragement and motivation can reinforce positive behaviors and modify negative behaviors, resulting in behavior modification.
“Gamification” uses game participation to reinforce good behaviors. For example, employers could introduce a weight-loss challenge to employees that drives positive behaviors, increasing participants’ likeliness of winning the game. Social media and other technologies, such as text messaging, can provide reminders and social connections to encourage positive behaviors, as well.
While compelling evidence is lacking, other alternative approaches may also improve recovery from stroke. These include:
Mind-body medicine may also help improve mindset and thus aid in recovery. These kinds of therapy include:
Some traditional medicines have been used to prevent or improve stroke complications. The active components in these herbs are not always known. Doses are also not regulated; therefore, standardized dosing is hard to establish. Speaking with a health care professional before taking any herbal medicines is best. Some herbal medicines that may benefit stroke survivors include:
The results of the studies that have been done on these botanicals are promising, but more research is needed to support their use in treating strokes.
About 4 in 5 strokes are preventable. You can also take steps to prevent recurrence and disability caused by stroke, though none of these is guaranteed.
A critical factor in preventing stroke is choosing a healthy lifestyle. Recommendations for adopting a healthy lifestyle include:
Medications can also help with stroke prevention if lifestyle changes are not enough. People with risk factors that can be managed by medication may be prescribed these drugs. These medications are:
The anticoagulants mentioned are newer and shorter-acting. Because of this, they usually do not require weekly blood tests and have a lower risk of bleeding complications, unlike their longer-acting counterparts.
Though these newer anticoagulants have benefits, there are situations where warfarin, a longer-acting anticoagulant, may be the better option. The National Institute on Neurological Disorders and Stroke suggests that warfarin is best for those with atrial fibrillation, those over the age of 65, or people with additional risk factors. Younger people with atrial fibrillation may have adequate protection from daily doses of aspirin.
Medically reviewed by Beverly Timerding, MD.
What topics would you like to read about? Please let us know at health@epochtimes.nyc