Migraines are a type of recurring headache that can be debilitating. Moderate to severely painful, their symptoms can vary as much as the pain. While migraines share similarities with other types of headaches, health care professionals can distinguish migraine headaches from other types.
This sometimes-disabling neurological disorder affects more than 1 billion people worldwide, according to a consensus statement published in Nature Reviews Neurology. In the United States, approximately 15 percent of people experience migraines. These severe headaches can disrupt a person’s daily activities and develop complications.
According to Cleveland Clinic, more than 150 types of headaches are divided into two groups: primary and secondary.
Migraine headaches are primary headaches, meaning another condition does not cause them. In contrast, secondary headaches are the result of another condition. There are three main types of migraines: migraine without aura, migraine with aura, and chronic migraine. An aura is one or more sensory disturbances that occur before migraine onset.
When the aura phase of a migraine does not occur, it is considered a migraine without aura. Some characteristics of this type of migraine are:
Migraines that contain the aura stage are migraines with aura. About 15 to 20 percent of people who have migraines will experience an aura. Auras can happen before you experience a migraine or during the migraine.
Besides the characteristics of the aura phase, more specific characteristics of auras are:
Chronic means long-lasting. In this case, a chronic migraine lasts more than 15 days per month for over three months.
People who experience chronic migraines may switch between chronic and episodic migraines, and those who experience episodic may switch to having chronic migraines.
People with a headache disorder, such as migraines, may develop chronic migraines due to the overuse of headache medication.
Less common types of migraines include:
Symptoms of migraine headaches can differ among the types of migraines. The most common symptoms (pdf) include:
If you are experiencing headaches, it is always best to see your health care provider to be diagnosed and eliminate any contributing conditions. According to Mayo Clinic, if you are experiencing any of these symptoms, see your health care provider soon, as a more severe condition may exist:
This list is not all-inclusive. If you experience any new or changed symptoms with your migraines, it is best to see your doctor for further guidance and to ensure another serious condition doesn’t exist.
Migraines do not affect everyone the same. How a person experiences migraines can be affected by age, gender, and physiology.
Older people more often have migraine aura without headache and more secondary headaches because of existing comorbidities and adverse events. Migraine symptoms change with age, as well. Older people are less likely to have nausea and vomiting but more likely to have neck pain. When people over 55 experience migraines, considering their comorbidities and medications is necessary to make a diagnosis.
For children experiencing migraines, bed rest may be enough to manage the migraine. Their attacks are often shorter, less pulsating, with prominent gastrointestinal disturbances. Children who experience migraines may see an increase in prevalence when they reach adolescence.
As mentioned above, children may experience two types of migraines not shared by others: basilar-type and abdominal migraines.
Although medications may help to manage migraines in children, consult a health care professional before administering any medications.
Due to various hormonal changes, women may experience migraines during menstruation, pregnancy, postpartum, menopause, and when taking oral contraceptives.
During pregnancy and when breastfeeding, women should avoid preventive treatment. Preventive medications carry to risk of harming the fetus or infant. While NSAIDs are considered safe during the second trimester of pregnancy, some health authorities also consider them safe during the first trimester. Consult your physician about taking medication while pregnant. According to the Nature Reviews Neurology consensus statement, migraine medications contraindicated during pregnancy are:
Women with menstrual migraines may benefit from long-acting NSAIDs or triptans when acute therapies are unsuccessful. Taking these daily for five days, starting two days before an expected period, may prevent the occurrence of menstrual migraines.
According to the Nature Reviews Neurology statement, women who experience migraine with aura should not take combined hormonal contraceptives. Doing so may increase the risk of stroke.
According to the American Medical Association (AMA), the exact cause of migraine headaches has yet to be confirmed. However, specific neurological issues are believed to contribute to migraines.
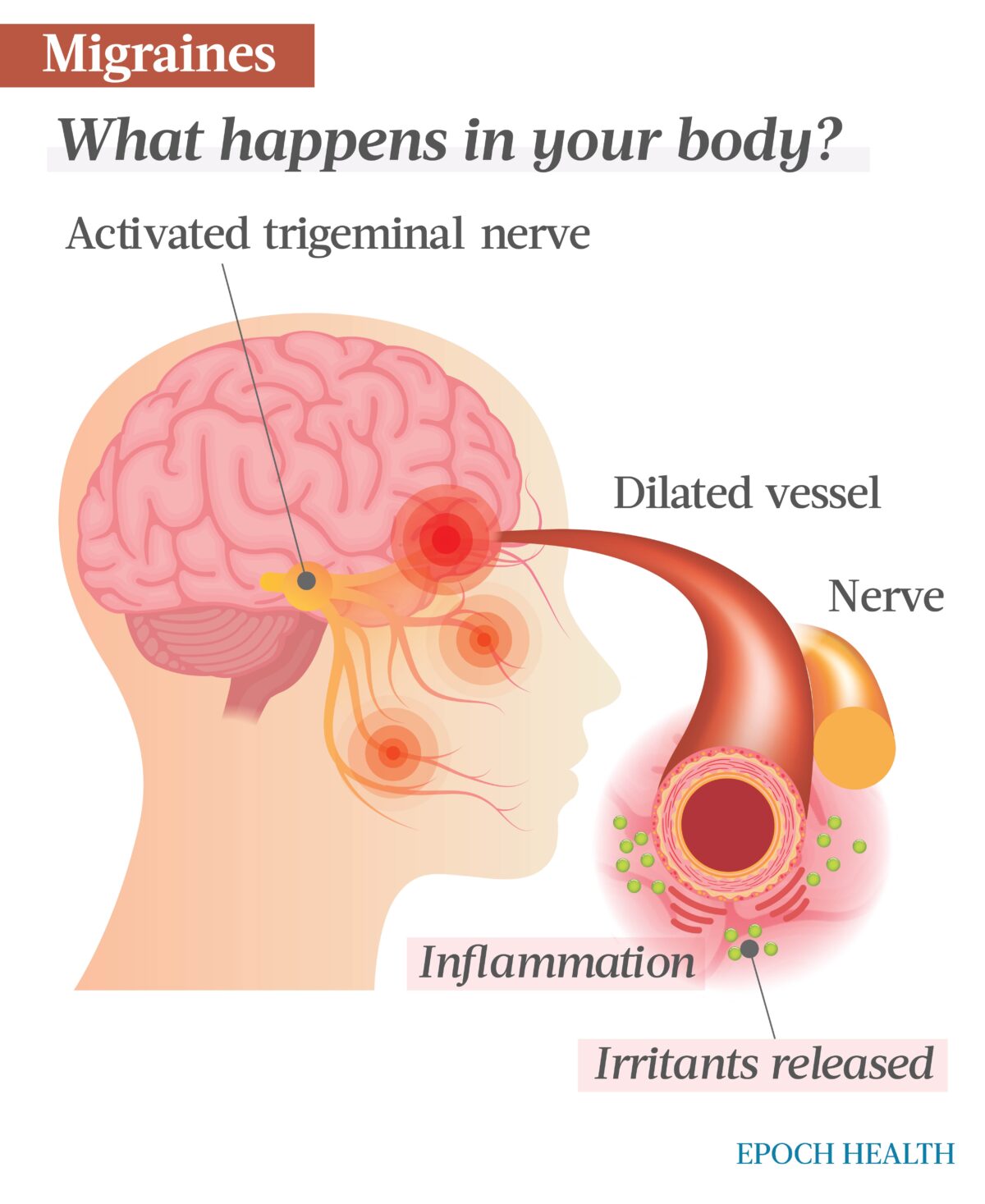
Issues in the nervous system may be a cause of migraines. According to Nature Reviews Neurology, migraines involve the peripheral and central activation of the trigeminovascular system. Changes in brain activity can lead to inflamed blood vessels surrounding the brain. Sudden changes in your body or environment may also cause migraines.
In contrast to migraines, secondary headaches occur because of another condition. The following conditions can sometimes be mistaken for migraines:
Triggers do not cause migraines. Instead, they activate the processes that cause migraines. When exposed to triggers, people prone to migraines may experience one soon after exposure. Not every trigger affects everyone prone to migraines, nor will everyone prone to migraines experience the same trigger. Possible triggers include:
A migraine has four stages, which Cleveland Clinic depicts in a helpful graphic:
- Prodrome
- Aura
- Attack
- Postdrome
Before a migraine occurs, even days before, you may experience changes to your body and personality. These can be warnings of an impending migraine and can include:
Auras may or may not occur with a migraine. When they do occur, they can happen before or during the migraine. An aura may include:
The attack is an active migraine. During this stage, you may experience any previously discussed symptoms, which may last for hours up to several days.
Symptoms occurring after the attack comprise the migraine’s postdrome, or final phase. These may include:
UC Berkeley states that migraines typically occur in people between 15 and 55. Women are three times more likely to experience migraines than men, and 70 to 80 percent of sufferers are likely to have a family history of migraines.
Additionally, people who experience high stress levels are more at risk of experiencing migraines.
While health care providers can diagnose migraines, it is best to prepare for your appointment first to make the diagnosis process easier. Prepare by keeping a headache journal, documenting your history of migraines in a calendar, and recording any family history of migraines. When documenting your headaches, include intensity, frequency, and duration.
Health care providers depend on a patient’s history of headaches and family history to diagnose a headache condition. The age you began experiencing the headaches and whether you have an aura can help determine if the headaches are migraines.
Headaches can be secondary, so this possibility must first be ruled out. To do this, your doctor will need a complete health history and may occasionally request neuroimaging.
The primary tool for diagnosing migraines is the patient’s headache history. Migraines are a clinical diagnosis, so there are no tests explicitly used to diagnose them.
To exclude causes of secondary non-migraine headaches, neuroimaging such as computed tomography (CT) scans or magnetic resonance imaging (MRI) may be used. For the same reason, a physician may order blood tests. The physician may also order an electroencephalogram (EEG) to rule out seizures.
Certain auras may also indicate migraine complications. An aura that persists for over a week but shows no signs of infarction is a persistent aura without infarction. On the other hand, a migrainous infarction is a condition in which a migraine lasts longer than one hour and shows correlating areas of infarction on CT scans or an MRI and would be associated with stroke symptoms. This is in contrast to the temporary, though often prolonged, one-side weakness seen in hemiplegic migraine that does not ultimately result in stroke. An emergent medical evaluation is needed to determine the difference.
While no causal link between seizures and migraines exists, some research suggests a relationship. People who have migraines are more likely also to have epileptic seizures.
The symptoms of migraines can also cause complicate a person’s daily life. This may come in the form of lost hours at work or a person being atypically inactive. The following complications can arise from chronic migraines:
There is no cure for migraines. Treatments for migraines help ease the symptoms, shorten the duration, or prevent frequent attacks. The most common treatments are medication and lifestyle changes.
Different kinds of medications may stop a migraine attack or its symptoms. Some medications quiet sensitive nerves and reduce inflammation.
Treating migraines is personal. Not every medication will produce the same results for every person. It is up to the health care provider and the patient to discover the best medications for the patient’s symptoms.
Medications for migraines can be OTC or prescription drugs.
Migraine treatment rarely requires the care of a specialist. For chronic migraines, a referral to a specialist may be necessary, as management of such migraines can be quite challenging.
According to the Nature Reviews Neurology paper, several medications are commonly used to treat migraines. Three lines of treatment divide these medications.
First-line: First-line medications for treating migraines are often OTC drugs. These can be taken two to three days before an anticipated migraine, as in menstrual migraines, or at the onset. Drugs used in this line include acetaminophen and NSAIDs like ibuprofen. Taking these at the start of the migraine may head off intensity and duration.
Second-line: Second-line medications are most often prescribed medications called triptans. They are most effective when taken early during an attack.
Triptan drugs include:
Also in this line is the combination of NSAIDs and triptans. If the single use of either of these drugs is not successful, combining them may be.
Third-line: When first- and second-line drugs are unsuccessful or contraindicated, third-line drugs are an option. This line contains ditans and gepants. Lasmiditan is the only ditan currently approved for acute migraine use. Ubrogepant and rimegepant are the only two gepants approved for the same use.
Other medications, such as antiemetics, treat nausea and vomiting that some people may experience with migraines. Many studies suggest that antiemetics such as metoclopramide also successfully relieve acute migraine pain.
Stress is a known trigger for migraines. Those under extreme stress or unable to manage stress may experience migraines. The experience of the migraine itself may cause emotional distress and suffering.
A person who experiences frequent migraines may become frustrated, sad, angry, or depressed. It is best to seek the help of a health care professional when experiencing these feelings.
While there are claims that some natural remedies may help manage migraines, the evidence is lacking. More research is required, but there are a few promising options.
Riboflavin, or vitamin B2, has been studied as a measure to decrease the frequency of migraines. Data are sufficient enough that the American Academy of Neurology and the American Headache Society believe riboflavin effectively prevents migraines.
The dose of riboflavin generally given is 400 milligrams daily for adults to prevent migraines. Consult your health care provider before taking this vitamin supplement to ensure you receive the correct medication and dose.
Feverfew is another natural remedy thought to prevent migraines. Though the data supporting this are lacking, preliminary studies are encouraging. Further research is needed to support the preliminary findings.
When using feverfew to prevent migraines, take it once daily for one month. If there is a decline in migraine attacks, your health care provider may slowly decrease the dose. Again, consult your primary health care provider before using natural remedies.
Feverfew is not recommended for pregnant women or those taking NSAIDs.
The American Headache Society and the American Academy of Neurology suggest magnesium may prevent migraines.
Magnesium in tablet form is available OTC. It can be a good preventative measure for those who experience migraine with aura, may be pregnant, or menstrually related migraine. The dosage is typically 400 to 600 milligrams per day. Consult your health care provider before taking magnesium to prevent migraines.
Butterbur may reduce the frequency of migraines in adults and children, according to the National Center for Complementary and Integrative Health (NCCIH). However, its safety is uncertain.
Some butterbur products contain pyrrolizidine alkaloids (PA), which may harm the liver, lungs, and blood circulation and cause cancer. Though some butterbur products claim to be PA-free, some question these claims.
It is best to be safe and discuss using butterbur with your health care provider to ensure it is safe.
The NCCIH also says that coenzyme Q10 shows promising preliminary data suggesting it decreases the number of migraine attacks in one month. Although it appears to have minimal risks, further research is needed.
Coenzyme Q10 may interact with medications such as insulin, anticoagulants, and chemotherapeutic drugs. As with all natural remedies, consult your primary physician before using coenzyme Q10.
Using ginger does not prevent migraines. However, it may minimize pain and reduce nausea. As such, it may be good to use ginger when these symptoms are present with a migraine.
While migraine prevention is possible, there remains no cure. People who experience migraines may learn to cope with the condition and seek support from health care professionals, family, and friends.
Common ways to cope with migraines include:
Preventing migraines is not always possible, but medications and lifestyle changes can reduce their occurrence.
The Nature Reviews Neurology paper states that prevention medication follows a three-step approach when treating migraines.
Beta blockers, anticonvulsives, and angiotensin II receptor blockers (ARBs) are classifications of drugs used in the first-line prevention of migraines. These medications include:
Take these medications daily to decrease the number of migraines you experience. Not all people will have the same experience when using these.
Anticonvulsants are also a classification used for second-line prevention of migraines, but the specific drug used is not the same as that in the first-line prevention medications. Along with anticonvulsants are antidepressants and calcium antagonist drug classes. Also taken daily, second-line prevention medications include:
Third-line migraine prevention medications are the last resort for decreasing migraine occurrence. This group has two classes of drugs: botulinum toxin and calcitonin gene-related peptide (CGRP) monoclonal antibodies. Medications from these two classes used for migraine prevention are:
These medications are all injections, and the frequency with which they’re taken differs. Some are taken monthly, while others quarterly. People using these often do not see results immediately.
Evaluating these medications’ efficacy should occur three to nine months after starting the medication. For this reason, consistency with dosing is essential. Inconsistency can negatively impact the drug’s effectiveness.
Your health care provider will sometimes pause medication use after six or 12 months to prevent overuse.
One way to manage living with migraines is to make lifestyle changes. Adjusting your lifestyle does not guarantee the frequency of migraines will decrease. Some adjustments may help, while others may not.
Lifestyle changes include:
Medically reviewed by Beverly Timerding, MD.