According to the U.S. Centers for Disease Control and Prevention (CDC), heart disease is the leading cause of death in the United States. One person dies every 34 seconds, making cardiovascular disease responsible for 1 in every 5 deaths.
“Heart disease” is a term used to describe a variety of conditions that affect the heart. These diseases include:
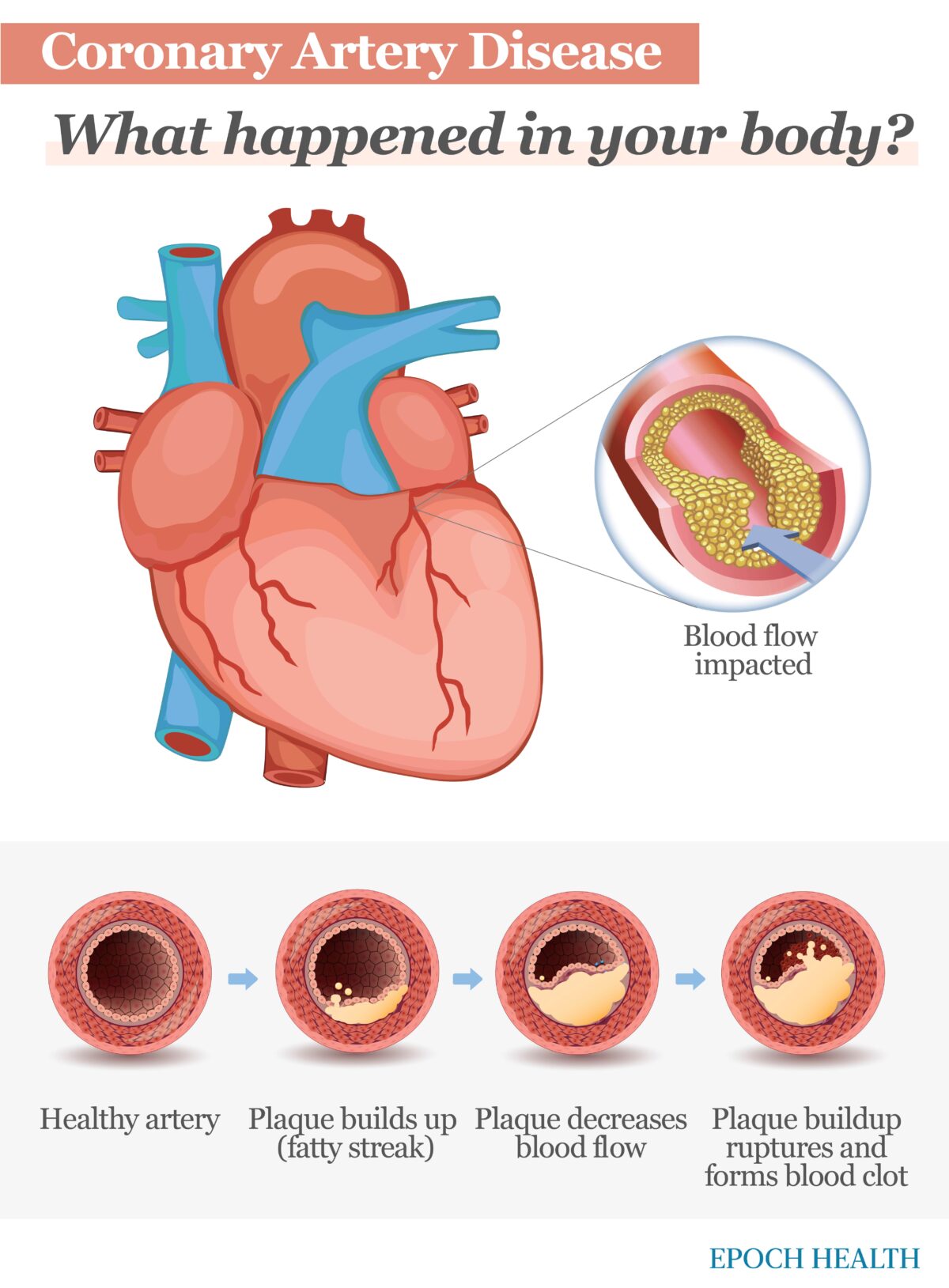
Coronary artery disease (CAD) is the most common type of heart disease in the United States, according to the CDC.
CAD is caused by the buildup of fatty deposits, also called plaques, in the walls of the coronary arteries—a process called atherosclerosis. The coronary arteries surround the heart and are responsible for supplying blood, nutrients, and oxygen to the heart muscle.
When these plaques build up inside the arteries, blood flow to your heart is decreased or becomes blocked. If a plaque ruptures, it may cause chest pain and discomfort, called angina, or a heart attack.
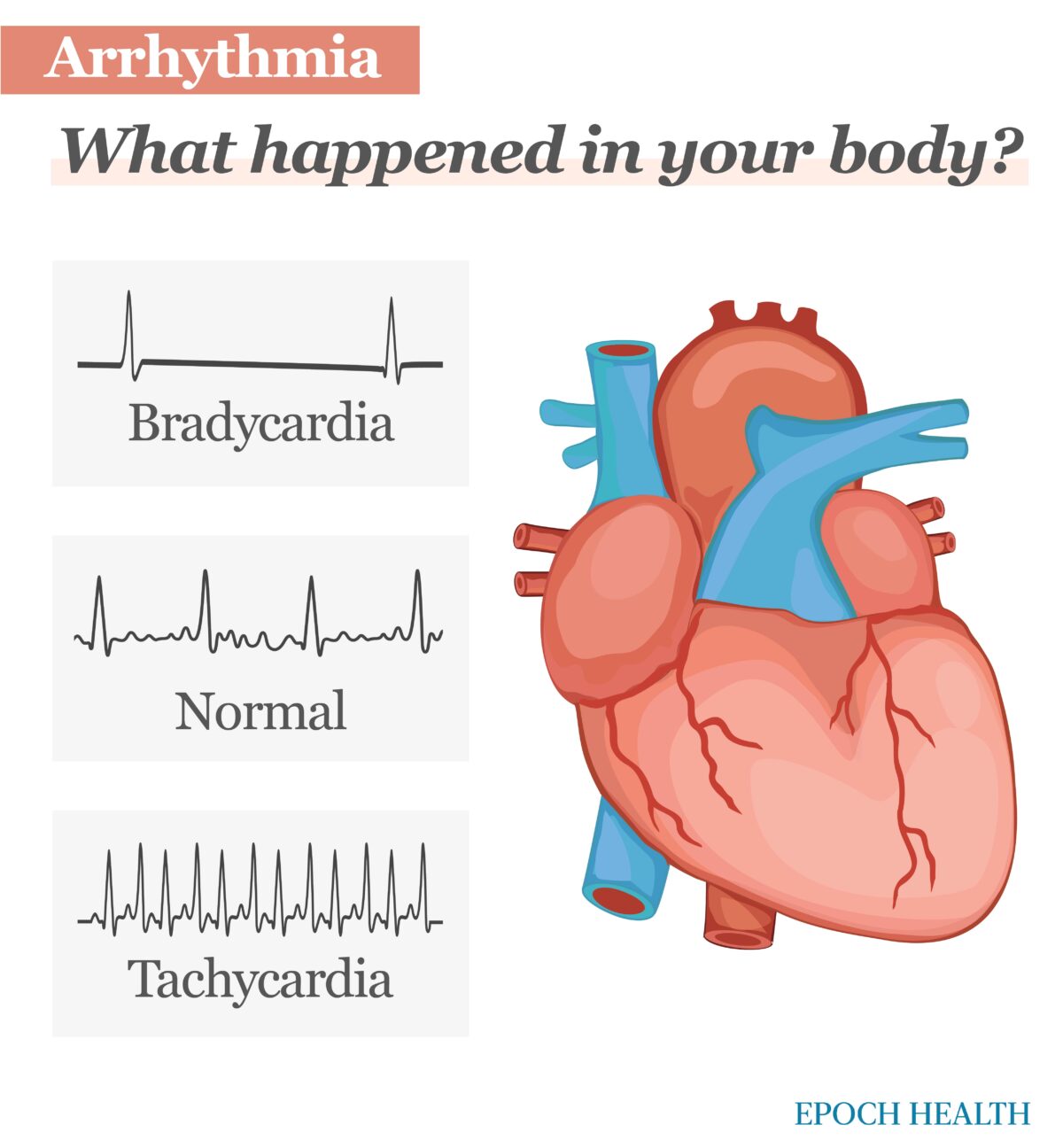
An arrhythmia is an irregular heartbeat. Arrhythmias arise when the electrical signals that direct heartbeats don’t function properly.
Many factors can cause arrhythmias, including congenital heart conditions that people are born with, such as tetralogy of Fallot or atrial septal defect.
Oftentimes, the cause of arrhythmia is unknown. However, heart or vascular conditions such as high blood pressure, cardiomyopathy, coronary artery disease, heart muscle changes, and heart valve disorders can lead to arrhythmias. Red wine, excessive alcohol use, and caffeine consumption can also cause arrhythmias. Recent studies also show that adults who use methamphetamines, cocaine, opiates, and marijuana may have a 35 to 86 percent higher risk for developing heart arrhythmias than those who do not.
Arrhythmias are usually grouped into two categories.
They are grouped by the speed of the heart rate:
And by location of the arrhythmia:
Congenital heart defects (CHDs) are abnormalities in the heart that present at birth. These anomalies could be present in the heart walls, valves, or blood vessels. In severe cases, blood vessels or heart chambers may be poorly formed, missing, or in the wrong place.
According to the peer-support program Mended Hearts, CHDs are the most common type of birth defect, affecting almost 1 percent of births.
While most causes of congenital heart defects are unknown, Mended Hearts reports that 15 to 20 percent of all CHDs are linked to known genetic conditions. Most are caused by a combination of genes and other risk factors including maternal conditions and environmental exposures.
Maternal conditions include elements such as smoking, some infections, and maternal obesity. Environmental aspects include factors such as the mother’s diet, maternal diabetes, and chemicals and medications.
Around 1 in 4 babies born with a heart defect has a critical congenital heart defect. These babies typically require surgery or other procedures within their first year of life.
Congenital heart defects are characterized by several different conditions. Those marked with an asterisk (*) are considered critical heart defects:
People with heart defects are faced with life-long risks of health problems such as issues with eating, growing, difficulty with exercise, developmental delays, heart failure, heart rhythm problems, sudden cardiac arrest, or stroke.
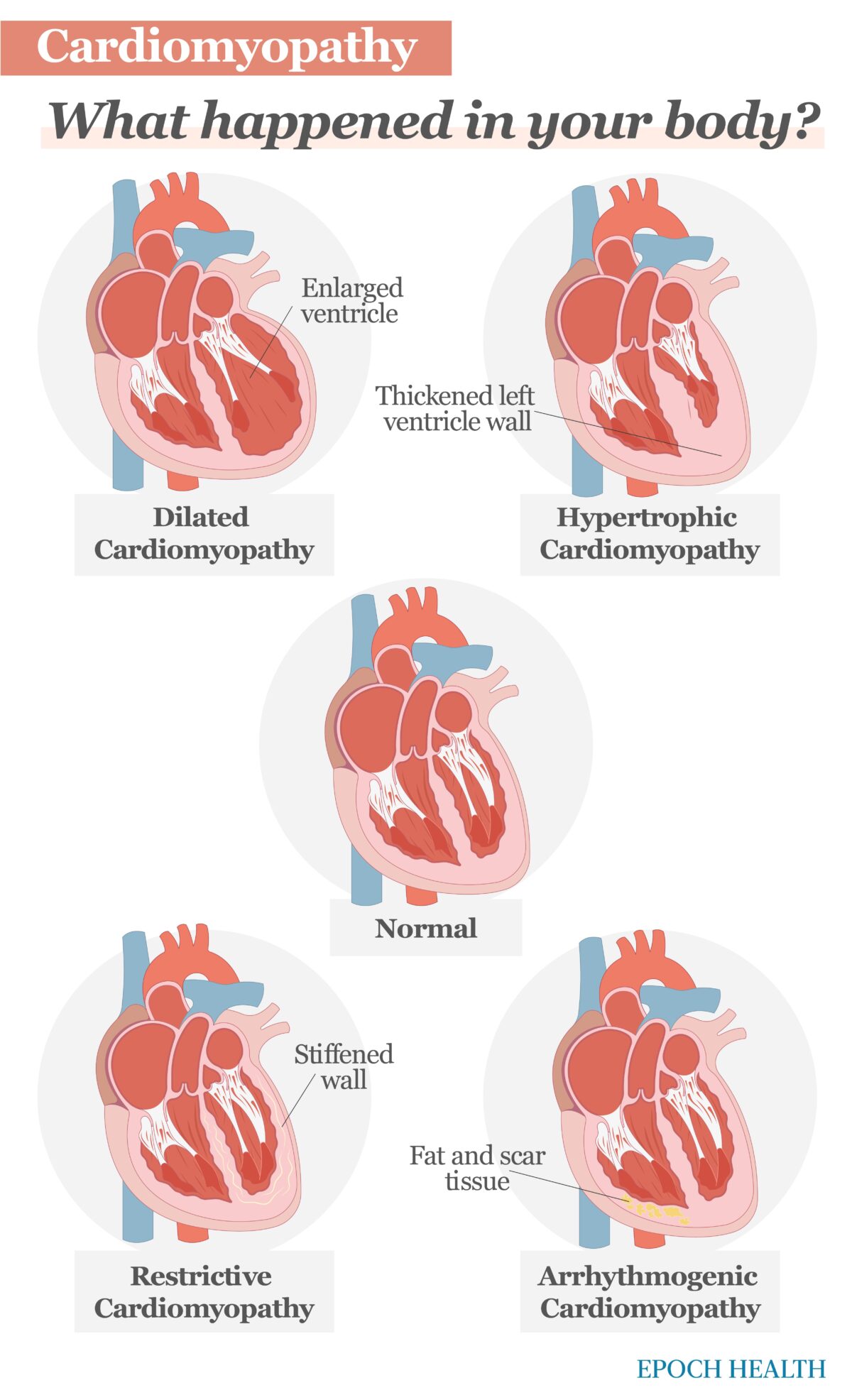
Cardiomyopathy is an inherited or acquired disease of the heart muscle that makes it difficult for the heart to pump blood. It is more common in men than women.
The cause of cardiomyopathy is often unknown. Yet in some people, the cause is the result of an acquired illness or an inherited condition passed on from a parent. These include the following:
Cardiomyopathy, which is linked to heart failure, is characterized by four main types:
Valvular heart disease is damage to, or a defect in, one or more of the four heart valves: the mitral, pulmonary, aortic, or tricuspid.
These four valves open and close to move blood through your body. The tricuspid and mitral valves regulate the flow of blood between the atria (upper chambers of the heart) and the ventricles (lower chambers of the heart).
Several things can damage the heart valves. A heart valve may not close properly, and the blood may leak backward (regurgitation), it may be narrowed (stenosis), or the valve may be formed improperly so there’s no proper opening for blood to flow (atresia). In these instances, the blood flow through your heart and into your body is disrupted.
Symptoms will differ depending on the type of heart disease.
Symptoms of coronary artery disease can include:
CAD may exhibit different symptoms in men and women. For example, men are more likely to have chest pain, while women are more likely to have other symptoms in addition to chest discomfort, such as nausea, shortness of breath, and extreme fatigue.
Heart arrhythmia symptoms may include:
Congenital heart defect symptoms in children could include:
Some of the less-serious congenital heart defects are often not identified and diagnosed until later in childhood or adulthood. Symptoms of congenital heart defects that don’t require immediate attention or usually aren’t life-threatening include:
With severity ranging from mild to severe, these birth defects can affect how blood flows through the heart and to the rest of the body.
Symptoms may not be present in the early stages of cardiomyopathy, but as the condition worsens, the following may appear:
Depending on which valve isn’t working correctly, heart valve disease symptoms typically include:
Endocarditis, an infection that affects the heart valves and inner lining of the heart chambers and heart valves (endocardium), could cause an array of symptoms:
Treatments may include medicine, surgical procedures, or a combination, and these differ among the types of heart disease.
Coronary artery disease generally requires lifestyle changes such as eating healthy, increasing exercise, and not smoking. Sometimes medications are needed. There are numerous drugs available to treat CAD, including:
CAD may require surgical intervention, such as angioplasty, stent placement, coronary artery bypass graft (CAGB), or off-pump coronary artery bypass surgery.
Occasionally, coronary artery disease is caused by an anomalous coronary artery. An anomalous coronary artery is an irregularity in the coronary artery, such as how it branches or how it’s shaped. If not treated, it can cause serious heart problems and even sudden death. Treatment involves angioplasty and stent placement to open up the blocked part of the artery.
If your arrhythmia requires treatment, your cardiologist will explain your best options and describe the risks and benefits of each one. Depending on your specific circumstances, choices might include medications, catheter-based procedures, or implanted heart devices such as internal defibrillators and pacemakers.
Two main types of drugs are used to treat heart arrhythmia:
Although surgery is often not a cure for congenital heart defects, many individuals require an operation(s) and/or medications in adulthood. In fact, according to Mended Hearts, about 25 percent of children born with a congenital heart defect will need heart surgery or other interventions to survive.
Congenital heart defect treatment is dependent on the seriousness and type of congenital heart defect you or your baby has. The majority of simple congenital heart defects will get better over time and generally do not require treatment at all.
Medication is often used if your baby has a particular type of congenital heart defect known as patent ductus arteriosus. Generally, patent ductus arteriosus goes away on its own. However, occasionally medicine is needed to close the patent ductus arteriosus in premature babies.
Indomethacin or ibuprofen causes the patent ductus arteriosus to constrict or tighten, which closes the opening. Acetaminophen is occasionally used to close patent ductus arteriosus.
Your provider will educate you on the need to change your diet, include daily physical activity, reduce stress, and avoid alcohol and drugs. Treatment options depend on the type and severity of cardiomyopathy with which you have been diagnosed.
Genetic types of cardiomyopathies cannot be prevented, but you can help control symptoms and complications by following a healthy lifestyle. If you have any underlying condition or disease that caused the cardiomyopathy, early treatment of that condition can help prevent it from developing.
These drugs combat irregular heartbeat, congestive heart failure, and high blood pressure that could further damage the heart or cause kidney damage. Examples of the medications used include digoxin, disopyramide, dobutamine, encainide hydrochloride, flecainide, fosinopril, ibutilide, and isoprenaline.
Surgical and nonsurgical procedures and devices used to treat cardiomyopathy might include:
Various types of devices can be surgically implanted in the heart to improve its function and reduce symptoms, including:
If a patient has only a mildly diseased heart valve without any symptoms, they generally don’t require treatment. However, they would need routine checkups to monitor the function and disease progression of the valve.
Treatment options include monitoring, medication, and surgical intervention.
Medication cannot cure heart valve problems, but it is used as a treatment modality. For example, anticoagulants (blood thinners) are used after receiving a prosthetic heart valve. Medication might also be used if a patient’s heart valve disease has led to other health conditions, such as increased blood pressure or heart failure.
When a heart valve can no longer perform its job, it may require replacement with an artificial valve. The procedure may have to be performed through open heart surgery. However, there are some instances where artificial heart valves can be implanted using a catheter.
There are two types of artificial heart valves:
- Mechanical prosthetic valves: These are artificial valves that are made out of metal or synthetic material. These mechanical valves last a long time and are generally used in younger people, although they aren’t used as much today as in years past. The disadvantage of mechanical valves is that blood clots may form and block the whole valve, or they could travel through the body in the bloodstream and cause a stroke. To prevent complications, people who have a mechanical prosthetic heart valve will need to take blood-thinning medication (anticoagulants) for the rest of their lives.
- Bioprosthetic (tissue) valves: These are replacement valves that are made out of biological tissue such as the heart tissue of pigs or cows. Those who have a bioprosthetic valve aren’t always required to take anticoagulants to reduce blood clotting. Bioprosthetic valves don’t last as long as mechanical valves and may require another surgery. These heart valves are typically used in people over the age of 60 or in younger people who aren’t able to take long-term blood-thinning medication.
In some young people, the aortic valve can be replaced with a different heart valve of their own. The valve between the right ventricle and the pulmonary artery, known as the pulmonary valve, is used to replace the diseased aortic valve. The removed pulmonary valve is then replaced with a bioprosthetic valve.
Although mitral valve regurgitation can also be treated with a prosthetic heart valve, the preferred treatment for the defective mitral valve is usually a repair rather than a replacement. This is done using a catheter procedure or through open heart surgery. This type of treatment is known as “heart valve repair.”
In a different procedure, a small metal clip is used to clip the flaps of the leaky valve together, helping the valve to shut properly.
Approximately 47 percent of all Americans have at least 1 of 3 key risk factors for heart disease. Key risk factors include high cholesterol, high blood pressure, and smoking. However, there are several other medical conditions, factors, and lifestyle choices that can place people at greater risk for developing heart disease. Those conditions include:
There are many different tests used to diagnose heart disease. Aside from chest X-rays and blood tests, the following studies may be used to diagnose heart disease:
Psychological factors are believed to play a significant role in the appearance and outcome of cardiac illness. Social and psychological factors and personality traits and characteristics are important factors that influence the morbidity of cardiovascular diseases (CVDs), according to an article published in Indian Heart Journal.
Personality in coronary artery disease has been studied over the last 40 to 50 years. Type A personality—illustrated by impatience, competitiveness, hostility, and dominance—is negatively related to the prevalence of cardiovascular diseases.
According to the Indian Heart Journal article, further studies have been conducted to survey traits that may influence CVD, such as:
Findings have been inconsistent; however, the debate about the role and significance of personality traits in the causation of CVDs continues.
Several natural remedies can help you minimize and better manage your risks of developing heart disease. While natural resources are helpful, it’s important to check with your doctor before incorporating them.
Vitamins and minerals taken in the correct doses may aid in lowering the risk of heart disease. Numerous studies, such as one published in the Journal of the American College of Cardiology (JACC), suggest a positive correlation between consuming vitamin and mineral supplements and heart disease prevention.
MBTs have emerged as the foundation in the treatment of heart failure, especially in cardiac rehabilitation programs. MBTs seek to reduce or suppress the high sympathetic nerve activity of heart failure by using practices that generate slow and deep respiration. These practices have also been proven to decrease cardiac events, lower blood pressure, and reduce atherosclerosis.
Dietary adjustments can be made, as well. The following items have promising effects for heart disease:
Schedule routine health screenings. High cholesterol and high blood pressure can damage the blood vessels and heart. If you don’t test for them, you won’t know if you have been afflicted by these conditions, or when additional medical attention is needed.
Heart disease is a leading cause of death, but it’s not unavoidable. While there are risk factors such as age, sex, or family history, there are multiple effective home remedies that you can implement to better manage your risks of developing heart disease.
Medically reviewed by Tia Delaney-Stewart, MSN-Ed, RN, PHN,CCM.