Alzheimer’s disease is a progressive disorder of the brain. Affecting approximately 6.5 million people ages 65 and older, the disease causes the brain to shrink and its cells to slowly die. Alzheimer’s is the most widespread cause of a gradual decline in thinking, memory, social, and behavioral skills.
Alzheimer’s disease is the seventh leading cause of death in the United States.
Alzheimer’s disease is classified into two types:
Early-onset Alzheimer’s disease, also known as young-onset Alzheimer’s, appears in people between their 30s and mid-60s. This type represents 5 to 6 percent of the Alzheimer’s population.
It is not fully understood why some people get the condition early on while others do not. For most people with early-onset Alzheimer’s, the cause is not related to any single genetic mutation.
Early-onset Alzheimer’s can result from mutations in one of three genes, APP, PSEN1, or PSEN2, which may be passed on to other family members. Combined, these genes are found in less than 1 percent of the overall Alzheimer’s population and approximately 11 percent of people diagnosed with early-onset disease. So if your parent or grandparent developed early-onset Alzheimer’s, one of these gene mutations may be involved.
The most common form of Alzheimer’s is late-onset Alzheimer’s disease. It surfaces in individuals in their mid-60s and accounts for 90 to 95 percent of Alzheimer’s cases.
A gene called apolipoprotein E (APOE), found on chromosome 19, has been commonly linked to late-onset Alzheimer’s. If you have this gene, it doesn’t necessarily mean you will develop the disease, but it suggests you are at higher risk.
APOE is characterized by three forms: APOE2, APOE3, and APOE4. APOE4 is the gene form that increases your risk of developing Alzheimer’s, and it typically means a slightly earlier onset of the disease is possible. A person could be affected by up to two types of APOE4 genes. The more APOE4 genes you have, your risk of developing the disease increases.
While APOE4 genes impact Alzheimer’s risk, the other elements that interact with genetics make it difficult to identify one specific cause of the disease.
Other genes could be involved with the development of late-onset Alzheimer’s, but these require additional study.
The signs and symptoms of Alzheimer’s disease will worsen with time and eventually become severe. People affected by early-onset Alzheimer’s may notice difficulty remembering conversations or recent events, but others do not usually notice these subtle changes. As symptoms progress, friends and family members will notice the changes.
Brain-related changes associated with the disease can impact:
As Alzheimer’s-related memory loss worsens, so does the patient’s ability to function in most settings.
People with Alzheimer’s may forget appointments, events, or conversations. They may repeat questions or statements and misplace items or put them in illogical locations.
As the disease progresses, Alzheimer’s patients may get lost in familiar places. They may have trouble choosing the best words to express their thoughts or converse, and they may eventually forget the names of friends, family members, and everyday objects.
Alzheimer’s causes difficulty thinking and concentrating. Abstract concepts, like numbers, are challenging for patients to navigate.
Everyday undertakings such as paying bills on time, managing finances, and carrying out multiple tasks simultaneously are incredibly challenging for patients.
In the end, a person suffering from Alzheimer’s disease may be unable to manage or even recognize numbers at all.
Alzheimer’s patients experience a decline in their ability to make rational decisions regarding everyday situations and circumstances.
These patients may make poor decisions when choosing the appropriate clothes for the weather or making inappropriate choices in social settings.
Responding to everyday challenges may become increasingly difficult. For example, an individual may not make good choices while driving or know how to react to food burning on the stove.
As the disease progresses, routine activities such as getting ready for work or following a cooking recipe become problematic. In time, advanced Alzheimer’s patients forget how to perform basic tasks such as brushing their teeth or getting dressed.
Brain changes associated with Alzheimer’s can affect a patient’s behavior and mood. According to Mayo Clinic, symptoms may include:
Although Alzheimer’s causes significant changes in skills and memory, patients can retain some of their skills even as symptoms worsen. This is because skills are controlled by parts of the brain that are affected later in the disease process.
Preserved skills may include reading, writing, singing, performing, making art, and sewing.
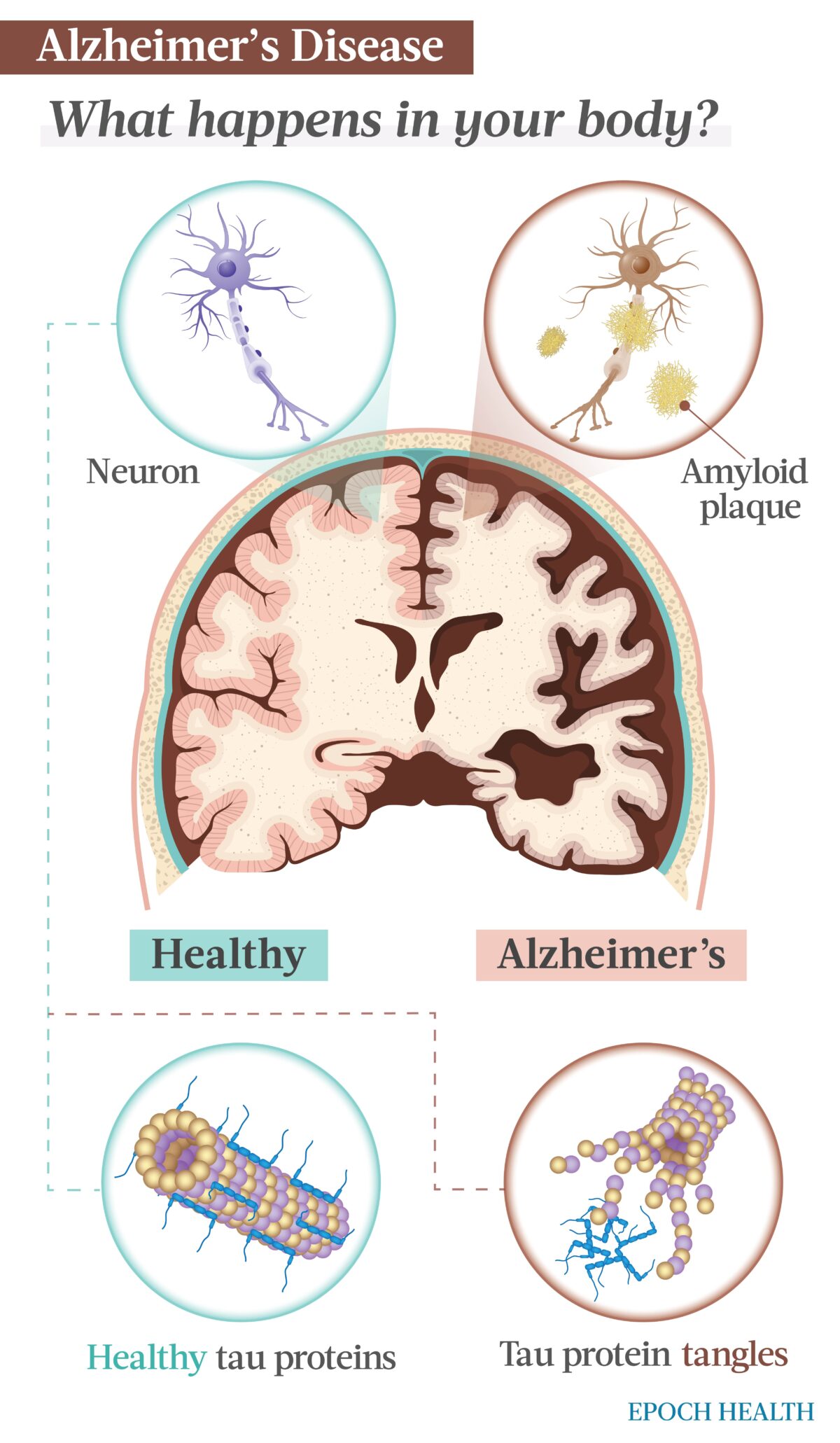
The precise cause of Alzheimer’s disease isn’t entirely known. It’s understood that brain proteins fail to function normally, disrupting the usual routine of brain cells, also called neurons. This initiates a series of events that damage the neurons, causing them to lose connection to each other and ultimately die.
Researchers theorize that for most people, Alzheimer’s is caused by a combination of lifestyle, genetic, and environmental factors that progressively affect the brain. However, from a genetic perspective, less than 1 percent of Alzheimer’s cases are caused by genetics that nearly guarantee a person will develop the disease.
Alzheimer’s disease begins years before the first symptoms appear. The damage usually originates in the part of the brain that controls memory. The loss of neurons begins to affect other brain regions in a fairly predictable pattern, and by the late stages of the disease, brain mass has diminished extensively.
Researchers are trying to uncover the role of two proteins in the development of Alzheimer’s:
As Alzheimer’s progresses, it eventually affects most brain areas and impairs language, judgment, problem-solving, memory, thinking, and movement.
According to Mayo Clinic, the disease is characterized by five stages.
Preclinical Alzheimer’s disease is the period when the disease begins but long before any symptoms are present. This stage is usually identified in research settings when the patient isn’t experiencing or aware of any symptoms.
This stage can last for years or even decades. Even though the patient isn’t experiencing symptoms or changes, technology can identify amyloid-beta protein deposits, an indicator of the disease. Identifying these deposits early may be important for future clinical trials as new treatments are developed for the disease.
Those with mild cognitive impairment experience changes in their thinking ability and memory. At this stage, changes have not begun to affect relationships and work. Those affected may find gaps in their memories, such as recent events or conversations.
People suffering from MCI may also have difficulty determining how many steps are needed to complete a task or judging how long the task will take. The ability to make solid decisions becomes harder during this stage.
Mild dementia due to Alzheimer’s disease is usually the stage in which most patients are diagnosed. During this stage, family, friends, and doctors fully realize that an individual is struggling with thinking, memory, and performing daily activities.
In this stage, patients may experience:
Moderate dementia patients are more forgetful and easily confused. As a result, they need assistance with self-care and daily activities, such as dressing and bathing.
Those suffering from moderate dementia may:
During this last stage of Alzheimer’s, mental function continues to diminish, and physical capabilities are further compromised.
In severe dementia, individuals may:
One in 10 people aged 65 and older has Alzheimer’s. Family history, age, genetics, infections, chemical exposure, and other factors play a role in who develops Alzheimer’s disease.
People with a parent or sibling who has been diagnosed with Alzheimer’s disease are at a higher risk of developing the disease.
As mentioned earlier, the APOE4 gene increases the risk of Alzheimer’s disease. However, while approximately 25 to 30 percent of the population carries an APOE4 allele, not everyone with this form of the gene develops Alzheimer’s.
Women are more likely to develop Alzheimer’s disease than men, according to Harvard Medical School. The main reason is that women appear to live longer than men. According to actuarial life tables, it’s likely that a baby girl born in 2019 will live five years longer than a baby boy born the same year: 81 versus 76 years.
Studies link air pollution to dementia and Alzheimer’s. According to Mayo Clinic, air pollution, such as smoke from burning wood and traffic exhaust, significantly increase risk.
Older age is the primary risk factor for Alzheimer’s disease. Although the disease isn’t a part of the typical aging process, your chance of getting the disease increases as you age.
According to Harvard Medical School, the following numbers of people develop Alzheimer’s each year:
There is evidence that traumatic brain injury (TBI) can lead to an increased risk of developing dementia or Alzheimer’s. The risk increases in individuals who have endured multiple or severe TBIs.
Alzheimer’s disease is common among people with Down syndrome. Scientists theorize this is likely related to having three copies of chromosome 21.
Chromosome 21 is a gene necessary for the production of the protein that leads to beta-amyloid creation. Beta-amyloid deposits can become plaques that damage brain tissue. Symptoms typically appear 10 to 20 years earlier in people with Down syndrome than in the general population.
People with MCI have an increased risk of developing dementia. If MCI mainly affects memory, progression to Alzheimer’s or dementia is more likely. If you are diagnosed with MCI, schedule routine appointments with your doctor to observe symptoms and progression.
Excessive alcohol consumption has been known to affect the brain. Studies suggest that heavy alcohol use is associated with an increased risk of dementia, particularly early-onset dementia.
Studies suggest that poor sleep patterns, such that individuals have trouble falling or staying asleep, are associated with an increased risk of Alzheimer’s.
Research shows that the same risk factors linked to heart disease may also increase dementia risk. However, whether these factors increase dementia risk by exacerbating Alzheimer’s changes in the brain or by leading to vascular changes there is unknown. Heart disease risk factors include:
These are all modifiable factors and can help lessen your risk of developing Alzheimer’s.
Engaging in activities and socializing arouses the mind and can help lower Alzheimer’s risk. Education seems to provide a similar effect. Education levels lower than high-school level are linked to Alzheimer’s risk.
A critical component in diagnosing Alzheimer’s disease is identifying a patient’s symptoms. Feedback from friends and family members about a patient’s symptoms and their impact on daily life helps medical providers make informed decisions.
Imaging studies and blood tests can help rule out other potential diagnoses, or they may assist your provider in identifying disease-causing dementia indicators.
Diagnosing Alzheimer’s disease typically involves physical and neurological exams and lab tests.
Your physician will begin your Alzheimer’s screening by performing a neurological physical exam examining various factors, including:
Your physician may conduct a brief mental status assessment to evaluate thinking skills and memory. Extensive forms of this test may provide greater detail about your cognitive function that may be measured against people of a similar education level and age.
These tests may help establish a diagnosis and serve as a baseline to track future symptoms.
Blood tests can determine whether other factors that can cause confusion and memory loss, such as low vitamin levels or thyroid disorder, are at play. Blood analysis may also be used to measure beta-amyloid and tau protein levels; however, these tests aren’t commonly available and may not be covered by insurance.
Brain imaging can identify visible changes related to Alzheimer’s and other conditions that may cause similar symptoms, such as tumors, trauma, or strokes.
Newer techniques may help identify specific changes in the brain caused by Alzheimer’s, but these are used primarily in clinical trials or major medical centers.
Imaging studies may include:
PET imaging may include:
Additional tests may sometimes be considered to measure amyloid and tau proteins in the cerebrospinal fluid. These are ordered if symptoms are worsening more quickly than usual or if dementia is affecting someone younger than the typical age.
The symptoms that characterize Alzheimer’s disease make it difficult for those inflicted to manage other health conditions.
According to Mayo Clinic, a person with Alzheimer’s may be unable to:
As Alzheimer’s advances, brain changes can lead to other conditions, such as:
Currently, no known treatment regimens will cure Alzheimer’s, but the U.S. Food and Drug Administration (FDA) has approved a few drugs to help control symptoms and manage disease progression. The majority of the approved drugs are most efficient in individuals who are in the early or middle stages of the disease.
Treating mild to moderate symptoms of Alzheimer’s can help provide patients with dignity, comfort, and independence for a longer duration.
Cholinesterase inhibitors improve cell-to-cell communication. Typically the first medications tried, these medications preserve a chemical in the brain that Alzheimer’s disease has diminished. As a result, patients will usually see modest symptom improvement.
The following medications are cholinesterase inhibitors that may help reduce or control behavioral and cognitive symptoms:
Lecanemab and aducanumab are immunotherapies that received FDA-accelerated approval to treat the early stages of Alzheimer’s disease. These drugs target the protein beta-amyloid to help decrease the amyloid plaques in the brain. In patients with mild cognitive decline, research demonstrated that lecanemab slowed the decline rate over 18 months and reduced the amyloid protein levels in the brain.
Studies conducted on aducanumab demonstrate its effectiveness in reducing amyloid protein in the brain too, but there is doubt regarding the drug’s ability to slow cognitive decline. Further research is underway to test both drugs’ ability to slow cognitive decline.
Patients diagnosed with moderate to severe Alzheimer’s are treated with an N-methyl-D aspartate (NMDA) antagonist called memantine.
This medication decreases symptoms, enabling patients to maintain some daily functions, such as using the bathroom independently, longer than they would have been able to without medication.
Memantine is believed to work by regulating an essential chemical in the brain called glutamate. Glutamate may be linked to brain cell death when produced in extreme amounts.
NMDA antagonists work differently than cholinesterase inhibitors, so these two drugs can be prescribed together.
Science has linked positive outlooks with better health outcomes. Those able to remain positive after an adverse life event seem to have better long-term health outcomes and lower rates of dementia.
A study published in the Psychological Science journal reported that people with a positive attitude are less likely to experience memory loss with age. Study participants reported the positive emotions they experienced over a month. During the final assessments, participants completed memory and performance tests. Tests involved recalling words immediately following their presentation and then again 15 minutes later.
Scientists studied the association between positive affect and memory decline while considering gender, age, depression, education, negative affect, and extraversion. Their findings showed that memory declined with age, but more positive individuals had less memory decline over 10 years.
Adopting lifestyle changes that support brain health and staying cognitively and socially active can help promote a better outlook and improved mood, as well as short- and long-term benefits for your brain.
Certain foods and supplements have proven beneficial in the management and prevention efforts against Alzheimer’s disease.
Brain-boosting foods that support memory, such as whole grains, legumes, fruits, vegetables, fish, and healthier fats, may help improve memory function. Mayo Clinic recommends the following foods to optimize memory function.
Complex carbohydrates such as cracked wheat, chickpeas, whole-grain couscous, and lentils are preferred brain food because they provide a sustained, slow supply of glucose. Neurons require glucose derived from carbohydrates to function properly. Whole grains and legumes take longer to metabolize and are high in B vitamin folate, which improves memory.
Watermelon is high in lycopene, a powerful antioxidant. In addition, it’s a great source of pure water, which is valuable to brain health. Even mild dehydration can reduce mental acuity and impair memory.
Grapes have an abundance of memory-enhancing compound resveratrol. Concord grapes contain polyphenols, an antioxidant especially helpful in the brain.
Berries, especially blueberries, have powerful antioxidants that protect the brain from oxidative damage, preventing early aging and memory loss.
Avocados are rich in monounsaturated fat. When consumed in moderation in place of saturated fats, these fruits improve memory function by helping lower cholesterol levels.
Dark, leafy greens, such as kale, spinach, and Swiss chard, can reduce age-related memory loss due to their antioxidants, such as vitamin C. Rich in folate, greens can improve memory by decreasing inflammation, which increases blood circulation to the brain.
Beets are rich in nitrates, natural compounds that dilate blood vessels to help more oxygenated blood enter the brain.
Crustaceans and shellfish are excellent sources of vitamin B-12, a nutrient believed to help prevent memory loss. Crustaceans and shellfish are high in cholesterol, so moderation is necessary.
Omega-3 fatty acids are great for brain health. Since these acids are mainly present in fatty fish, it’s suggested that fish should be added to an Alzheimer’s patient’s diet at least twice a week. Top picks include lake trout, sardines, salmon, light tuna, and anchovies.
Nuts are also a source of omega-3 fatty acids. These fats, found in foods such as walnuts, lower triglycerides, help moderate blood pressure, improve vascular health, and decrease the risk of blood clots.
Olive oil delivers monounsaturated fat. These fats help lower “bad” cholesterol levels when used instead of saturated or trans fats. In addition, extra-virgin olive oil improves vascular health and could play a role in early-onset Alzheimer’s prevention.
Turmeric: This common household spice contains the antioxidant and anti-inflammatory compound curcumin, known for its ability to boost brain tissues. Studies suggest curcumin may slow the progression of Alzheimer’s by reducing the number of plaques in the brain. Additionally, it may also prevent the buildup and clumping of beta-amyloid proteins.
Seeds containing essential nutrients: Consuming seeds such as pumpkin, sunflower, and sesame that are abundant in vitamin E and other essential nutrients is one of the most effective natural remedies for managing Alzheimer’s disease. This seed group is thought to enhance cognitive capabilities and support neural functions. Additionally, sesame seeds are a rich source of the amino acid tyrosine—a dopamine producer—and zinc, vitamin B6, and magnesium. They can help keep memory keen and the brain alert.
Ashwagandha (Withania somnifera): Widely used in herbal formulations to treat brain-related conditions, this herb is best known for its ability to provide nutrition to neurons.
Gotu Kola (Centella asiatica): A candidate for being a natural treatment for Alzheimer’s, this herb may improve blood circulation, support metabolism, enhance memory, and maintain a healthy brain.
Sesame seeds: A rich source of amino acid tyrosine—a dopamine producer—as well as zinc, vitamin B6, and magnesium, these seeds can help keep memory keen and the brain alert.
Alzheimer’s is not a preventable disease. However, numerous lifestyle risk factors can be modified to help lower your risk of developing the condition.
Research suggests that implementing measures to reduce the risk of cardiovascular disease may also lower your risk of developing dementia.
Heart-healthy lifestyle choices that may help reduce the risk of dementia include:
A large, long-term study conducted in Finland found that making lifestyle changes helped reduce cognitive decline among individuals at risk of developing dementia. Study participants were given individual and group sessions focusing on exercise, diet, and social activities.
Another study conducted in Australia measured coaching sessions, exercise, diet, and other lifestyle changes. Those individuals had better cognitive results after one, two, and three years compared to those who didn’t receive coaching support.
Other studies have shown that staying mentally and socially engaged is not only associated with a decreased risk of developing Alzheimer’s disease but is also linked to preserved thinking skills later in life. Staying socially and mentally engaged includes activities such as dancing, creating art, playing board games, reading, and playing musical instruments, among other activities.
Medically reviewed by Beverly Timerding, MD.