An especially severe form of monkeypox has been found by researchers to have a higher risk of severe complications and death among men with advanced HIV or AIDS, according to a study published in The Lancet.
According to the research team, monkeypox, or mpox, has had a considerable impact on men who have HIV and low CD4 cell counts. The current evidence also shows that all 96 monkeypox deaths have occurred only in people with HIV.
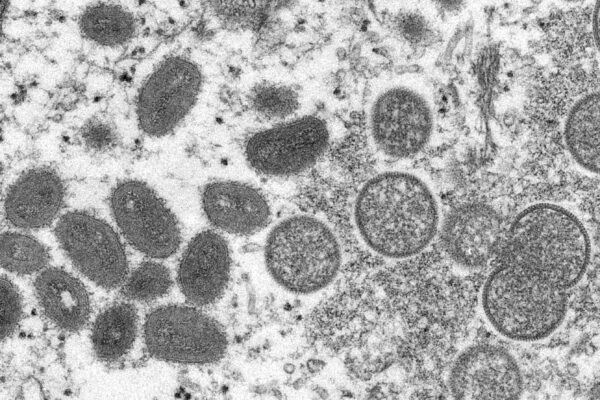
The researchers named the severe form of monkeypox “fulminant mpox,” and found that it caused large, decaying sores on the skin and genitals, and sometimes even the lungs. The study’s lead author, Oriol Mitja of Spain’s Germans Trias i Pujol University Hospital, shared graphic images of the severe disease on Twitter.
Patients with the lowest count of CD4 cells, which are a type of white blood cell that indicates a patient’s immune system’s health, typically had the most severe lesions and other symptoms, according to the study.
HIV destroys CD4 cells. A person without HIV is considered healthy if their CD4 count is above 500 cells per cubic millimeter of blood. People are diagnosed with AIDS when their CD4 count is below 200, according to the U.S. Centers for Disease Control and Prevention.
While monkeypox has historically been prevalent in several African countries, it began spreading globally in May 2022 largely among men who have sex with men. The study highlighted the importance of early diagnosis and treatment in this vulnerable population.
According to data from the World Health Organization, there have been more than 86,000 confirmed cases of monkeypox across 110 countries since the outbreak began, resulting in 96 deaths as of Feb. 22.
The research team looked at what happens when people with HIV and low CD4 cell counts (less than 350 cells per cubic millimeter) get monkeypox, and what the effects are.
The study revealed that individuals with HIV, mostly men, have made up 38–50 percent of the total number of cases in the 2022 multi-country outbreak of monkeypox.
Most reported cases were in people with high CD4 cell counts and similar outcomes to those without HIV. However, the study shows that people with more advanced HIV have worse clinical outcomes and higher mortality rates.
Mitja said the researcher’s first recommendation is that “every person with mpox should be tested for HIV,” and that everyone who has both HIV and monkeypox should be tested to measure their immune system to determine if they need intensive treatment.
He warned that the virus “doesn’t stop” and that some of the patients asked to be sedated because the pain was severe and “equivalent to those of a major burn.”
An international team of clinicians from 19 countries provided data on confirmed monkeypox cases between May 11, 2022, and Jan. 18, 2023, in people with HIV infection.
The data from 382 cases were included in the study, which consisted of 377 men and four women. The total number of men includes some who identify as women.
The median age of individuals included was 35.
At the time when the individuals were diagnosed with monkeypox, 349 of them were known to be living with HIV, 228 of whom were undergoing antiretroviral therapy (ART), according to the study.
The study found that the average CD4 cell count of people with monkeypox and HIV was 211 cells per cubic millimeter, with 85 individuals having a count of less than 100 cells per cubic millimeter and 94 with 100–200 cells per cubic millimeter.
Out of all the individuals, 193 had a viral load that was undetectable. Having an undetectable viral load means that the amount of HIV in a person’s blood is so low that it cannot be detected by standard blood tests. This doesn’t mean the person is cured of HIV, but that the virus is being effectively suppressed by ART, which greatly reduces the risk of transmitting HIV to others and also slows the progression of HIV disease.
Severe complications were found by the research team to be more common in people with a CD4 cell count of less than 100 cells per cubic millimeter than in those with more than 300 cells per cubic millimeter.
These complications included necrotizing skin lesions (54 percent versus 7 percent), lung involvement (29 percent versus 0 percent) occasionally with nodules, and secondary infections and sepsis (44 percent versus 9 percent).
Overall, 107 of the 382 individuals were hospitalized, of whom 27 died.
All deaths occurred in people with CD4 counts of less than 200 cells per cubic millimeter. Among people with CD4 counts of less than 200 cells per cubic millimeter, more deaths occurred in those with high HIV viral load.
An immune reconstitution inflammatory syndrome to monkeypox was suspected in 21 of 85 people initiated or reinitiated on ART, of whom 12 died.
A total of 62 individuals received tecovirimat and seven received cidofovir or brincidofovir. Three individuals had laboratory confirmation of tecovirimat resistance.
According to the study, a severe necrotizing form of mpox in the context of advanced immunosuppression appears to behave like an AIDS-defining condition, with a high prevalence of fulminant dermatological and systemic manifestations and death.
The researchers suggested that the severe form of monkeypox be included in the list of “AIDS-defining conditions” that international public health agencies maintain. This list helps doctors recognize which infections may pose the greatest risk to people with HIV.