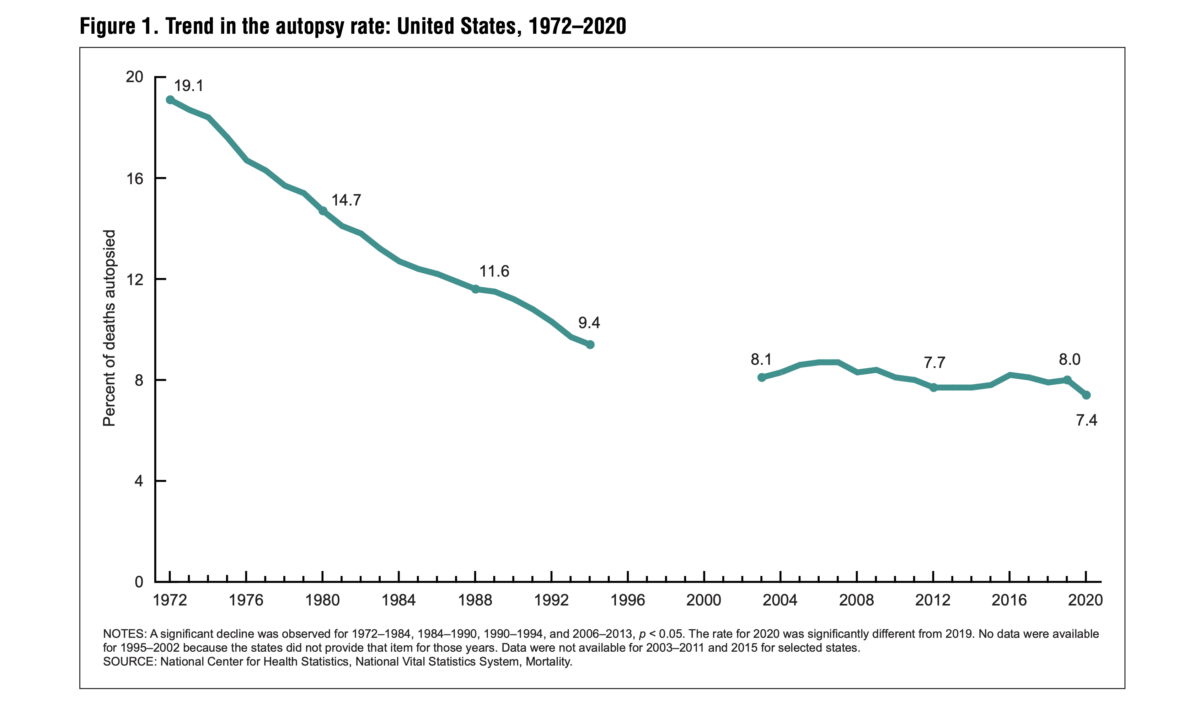
The autopsy rate in 2020 reached a record low of 7.4 percent, marking the lowest rate between 1972 and 2020, according to a recently released new report by the National Center for Health Statistics (NCHS), a subagency under the U.S. Centers for Disease Control and Prevention (CDC) (pdf). In 1972, the autopsy rate stood at 19.1 percent, but it has since experienced a steady decline.
The decline in autopsy rates hitting a new low in 2020 is concerning as it hampers diagnostic accuracy, limits medical research and public health understanding, impairs legal and forensic investigations, hinders quality assurance and education, and deprives grieving families of closure and answers about their loved one’s cause of death.
The report distinguishes between two types of autopsies: hospital or clinical autopsies requested by families or doctors to determine the cause of death and medicolegal autopsies ordered by legal officials to investigate death circumstances.
It notes the stability of autopsy rates from the 1950s to the early 1970s.
Between 1972 and 2020, hospital autopsies declined, while medicolegal autopsies remained stable or increased. Notably, in deaths caused by external factors like drug overdose, homicide, or suicide, the autopsy rate rose from about 19 percent in 1972 to 60 percent in 2020.
In an email to The Epoch Times, the NCHS noted that the distinction between medicolegal autopsies and autopsies for deaths from external causes is not clear, suggesting that the increase in external-cause autopsies may reflect the rise of medicolegal autopsies, while “hospital autopsies” may refer to autopsies on deaths resulting from diseases.
The report attributed the decline in autopsy rates to the removal of the 20–25 percent autopsy rate requirement in hospitals set by the Joint Commission on Accreditation of Hospitals in 1971.
Two other possible reasons are doctors’ reluctance to order autopsies, fearing potential lawsuits (pdf) if errors are discovered, even though such occurrences are relatively rare, and perceiving them as less valuable (pdf) due to advancements in medical technology, as described in a perspective published in Circulation.
The lack of reimbursement and diminishing academic importance are the two primary reasons for the consistent decline over the past 50 years, Dr. Harry Sanchez, director of Autopsy Service in the Department of Pathology at the Yale School of Medicine, told The Epoch Times.
Sanchez said that shortly after Medicare and Medicaid came into being in 1965, pathologists couldn’t bill an autopsy to the patient or the insurance company because it was no longer considered an individual procedure.
Autopsies are considered part of the hospital’s administrative and quality assurance work, covered by Medicare. “You get the same payment whether you do one autopsy or 100 autopsies,” Sanchez said. “So there’s really no financial incentive for the hospital to do more autopsies,” he added. “Likewise, you know, for pathologists, you can’t bill for the autopsy. So there’s no reimbursement to the pathologist who does the autopsy.”
Before the implementation of Medicare, autopsies were typically billed as a fixed proportion of the total medical bill, according to a 1980 report.
Autopsies involve significant work, with a routine adult autopsy alone taking a few hours. However, pathologists do not receive direct reimbursement for their efforts, including examining slides and generating reports.
The declining academic importance of autopsies has been influenced by significantly increased federal funding for medical research since the 1950s. As grant money became the primary measure of academic success, pathologists showed less interest in autopsies, focusing more on research. “There was increasingly less incentive to engage in things like quality assurance and teaching,” Sanchez said. “That continues to be true today.”
The federal budget for medical research rose from $3 million to $76 million between 1941 and 1951.
In the 1940s and 1950s, the autopsy rate was approximately 50 percent of all hospital deaths. By the mid-1960s, it had declined to around 25 to 35 percent.
“Very few pathologists want to do autopsies,” Sanchez said. “The incentives are just not there for them to change their minds … Economically and professionally.”
Autopsies have long been regarded as the gold standard in investigating the cause of death, accurately determining the cause and manner in most cases.
Even with today’s advanced medical technologies, Sanchez said, autopsies remain “the gold standard for seeing whether or not you made the right diagnosis.”
They hold immense importance for families, settling disputes when questions or doubts arise regarding a loved one’s death. Autopsies also play a crucial role in medical education and quality assurance within hospitals, Sanchez added.
Widely cited studies from 1960 to 2010 mentioned in the Circulation perspective have shown that autopsies uncovered Class 1 errors in approximately 10 percent of cases. These errors involve crucial causes of death that were initially missed by clinicians and where appropriate treatment could have impacted survival.
Sanchez also said that autopsies had proven particularly important from a public health standpoint. Cases involving the severe acute respiratory syndrome (SARS) caused by a coronavirus first reported in Asia in 2003 and the 2015 Zika virus epidemic and its association with microcephaly (when a baby’s head is much smaller than expected) all demonstrated the importance of autopsies.
According to the NCHS report, the COVID-19 pandemic led to a significant decrease in autopsy rates, particularly for COVID-19 deaths. The autopsy rate for COVID-19 deaths in 2020 was only 0.9 percent.
Many autopsy services were “essentially shut down” in early 2020, Dr. John Sinard, vice chair and director of clinical operations of the Department of Pathology at Yale School of Medicine, told The Epoch Times.
One reason was the “initial uncertainty about the mechanisms of transmission and thus the risk an autopsy might pose to staff performing the autopsy,” Sinard said.
Another reason was the shortage of personal protective equipment (PPE) for health care workers. “Many places elected to save PPE for live patient care,” he added.
Experts, including Sinard, acknowledged the importance of conducting more autopsies during the pandemic to gather crucial information about COVID-19, its effects on organs, and the causes of death. They believe that autopsies could have played a vital role in improving patient care and developing effective treatment strategies.
“It was really important to do autopsies in those cases so that people could find those things out,” he added, and “come up with rational therapies and stop doing things that didn’t work.”