Irritable bowel syndrome (IBS) is a common condition affecting 5 to 10 percent of the global population. Characterized by intermittent abdominal pain along with diarrhea, constipation, or alternating episodes of both, the disorder targets the gastrointestinal tract which includes the stomach and intestines. While IBS is a chronic condition that requires long-term management, it doesn’t produce changes in bowel tissue or increase your chances of developing colorectal cancer.
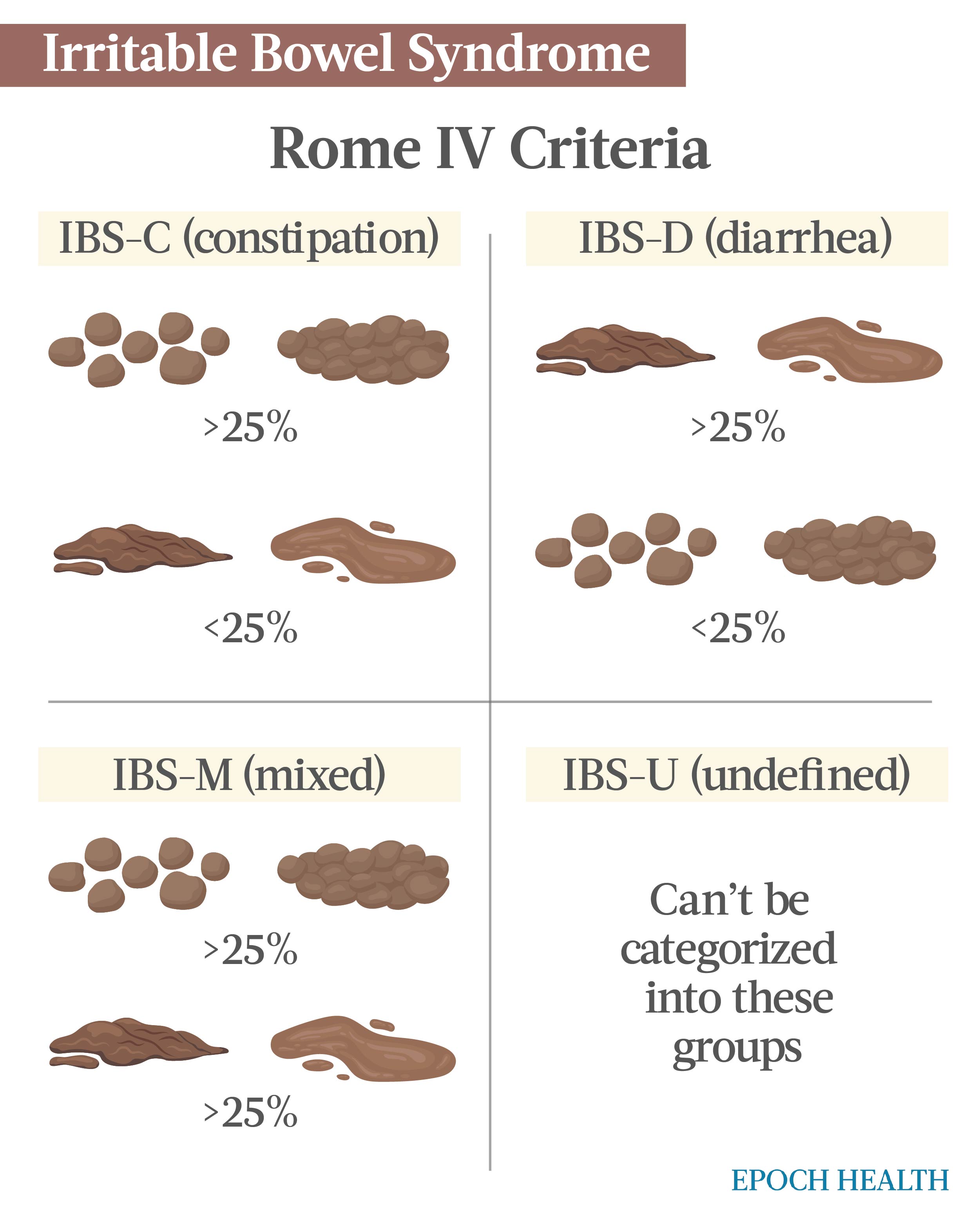
IBS is categorized into four types, each defined by the group of symptoms a person with IBS might experience.
IBS with constipation (IBS-C) is a chronic condition classified by abdominal pain and bloating, gas, and constipation. People suffering from the disorder may experience straining or difficulty having bowel movements, feel as if they are unable to empty their bowels, or have the sensation of needing to go to the bathroom but are then unable.
IBS-C is typically defined by hard pellet-like bowel movements and a change in either frequency or consistency, and its cause is unknown. Researchers believe there are several factors that could act as catalysts:
IBS-D is a multifactorial condition characterized by recurrent abdominal discomfort or pain and altered bowel function. Approximately one-third of the people diagnosed with IBS have the syndrome associated with diarrhea.
Factors such as prior gastroenteritis, changes in the gut microbiome, stress, bile acids, and short-chain fatty acids that alter gastrointestinal function can contribute to these IBS symptoms.
IBS-M is a type of irritable bowel syndrome that is characterized by inconsistent bowel habits. Individuals affected by this subtype will experience all of the typical IBS symptoms but will also be challenged by bouts of constipation and diarrhea.
IBS-M is defined by hard, lumpy stools for over 25 percent of bowel movements on symptomatic days, and loose, mushy stools for over another 25 percent of bowel movements on symptomatic days.
Stool changes can occur over the span of hours or days, while the main bowel difficulties can fluctuate between weeks or months of constipation and weeks or months of diarrhea.
IBS-U is a subtype of irritable bowel syndrome where the main symptoms of IBS are present, but symptoms and patterns vary. More research needs to be done on this subtype to flesh out its profile.
IBS is a chronic condition. Although symptoms vary, the most common include:
IBS patients may experience recurring episodes of abdominal discomfort or pain along with diarrhea, constipation, or a mixture of the two.
Logging a symptom journal where you can outline the food and quantities you have eaten will help you determine what foods trigger your symptoms. It’s important that you also document any symptoms that you experience after eating.
Patients should look for patterns in their tracked diet and symptoms to identify if certain foods improve or worsen their symptoms. When food triggers are identified, it’s important to cut back or eliminate one food at a time to know which food may have been triggering your symptoms.
IBS-C is triggered by various elements such as stress, certain foods, and hormones. Although the role of food allergies or intolerance isn’t entirely understood, many people affected by IBS experience increased symptoms after consuming particular food and drinks. Symptoms include:
Symptoms are often managed with diet and lifestyle changes. However, more severe cases will need to be treated with medication and counseling.
IBS-D symptoms include:
These can be triggered by numerous factors such as foods, beverages, stress, anxiety, and depression. While stress, anxiety, and depression do not cause IBS, they can lead to or worsen diarrhea symptoms. It’s important to find an effective way to manage your mood and stress levels.
Drinks with caffeine, carbonated drinks, alcohol, chocolate, sorbitol, dairy products, and fried foods may worsen IBS-related diarrhea. People challenged by IBS-D will also want to closely monitor fiber intake. While fiber is helpful for patients suffering from IBS with constipation, too much fiber could worsen symptoms for patients afflicted by IBS with diarrhea.
Vegetables, fruits, whole grains, and beans can also worsen diarrhea symptoms. IBS-D patients may need to experiment and track these foods in a food journal to identify what agrees with their stomachs.
IBS-M symptoms include:
IBS-U symptoms may include any of the common IBS symptoms, with varying patterns.
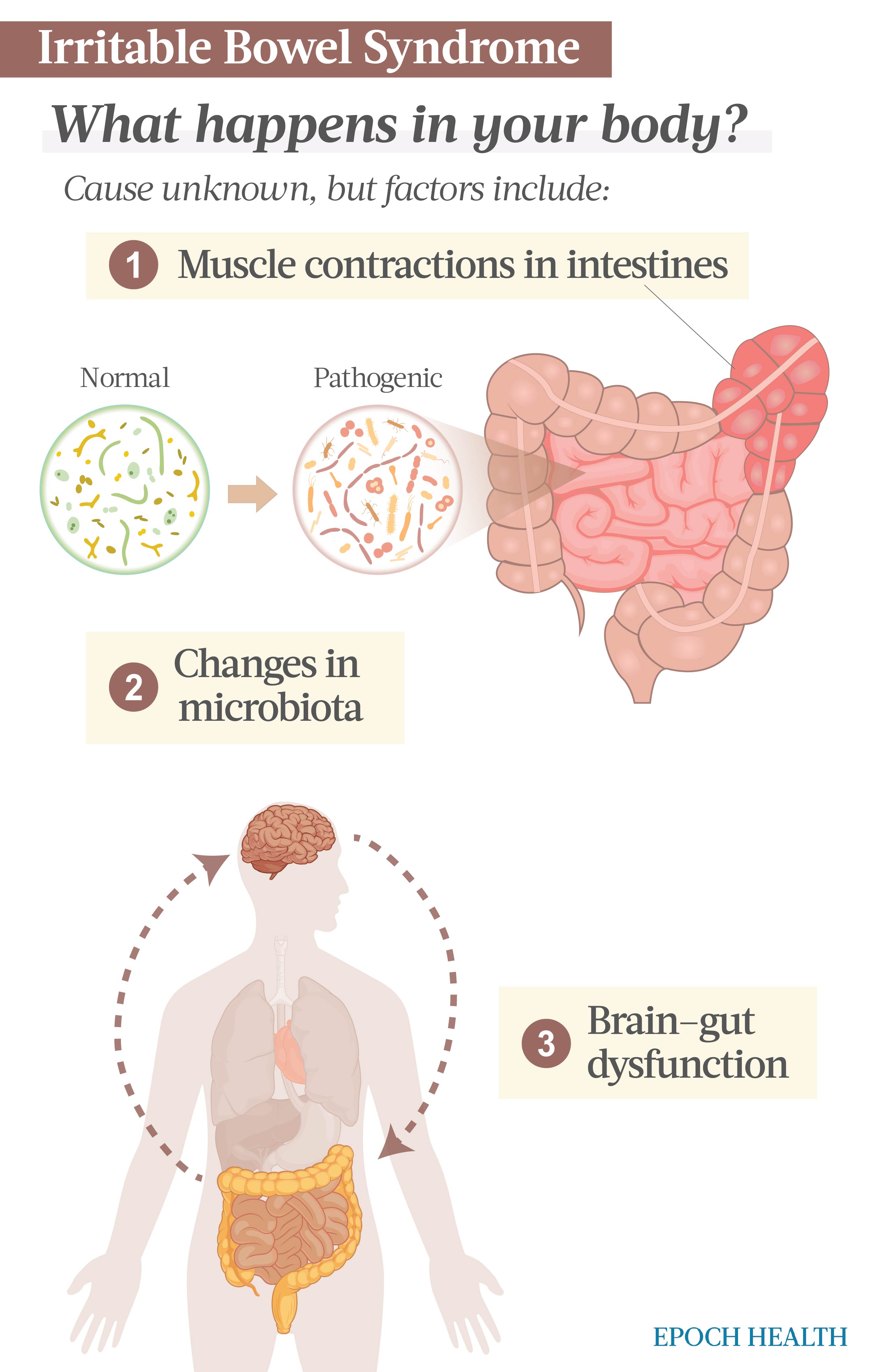
While a specific cause of IBS hasn’t been identified, several factors are thought to play a role in the condition and its progression. These factors include:
Most people have occasional symptoms of irritable bowel syndrome, but there are several factors that increase the probability of a person developing the syndrome. Such factors include:
There are no tests available to conclusively diagnose IBS. To determine if you have developed the condition, your physician will obtain a complete medical history, perform a physical exam, and order tests to rule out other conditions, such as inflammatory bowel disease (IBD) and celiac disease.
Subtypes of IBS are diagnosed by applying values known as the Rome IV Criteria.
The subtypes are based solely on the days an abnormal stool occurs.
Rome IV stipulates that symptoms have been present for the previous three months, with the original onset at least six months before irritable bowel syndrome was diagnosed.
If the initial assessment of IBS is not enough, your physician may order additional tests to check for other more serious conditions or to check for bacteria or infection.
Complications of IBS are limited, but they can have a significant impact on your daily life. Complications include:
Treatment for IBS is based solely on relieving symptoms. Mild symptoms are often relieved by managing stress and making lifestyle and diet changes. Diet and lifestyle changes include:
Upon evaluation, your doctor might also suggest that you eliminate certain foods from your diet:
Based on your diet, your physician may recommend supplements and/or medication management to further support symptom relief. These recommendations might include:
In severe cases of IBS or when other treatment modalities have failed, your physician may recommend medications that were specifically designed and approved for IBS. These medications include:
While it’s not clear how anxiety, stress, and IBS are linked, research suggests these conditions can and do develop together. A recent study conducted by the University of Missouri School of Medicine proved a correlation between mental health and IBS.
Diagnoses such as depression, anxiety, and suicidal ideation were amongst the most prevalent disorders. To improve the overall health of an IBS patient, this research suggests there is a greater need for health professionals to assess and treat psychiatric co-morbidities in their IBS patients.
This study analyzed more than 1.2 million IBS patients hospitalized across the United States over a three-year period. Of the participants, 38 percent also suffered from anxiety and over 27 percent had documented depression. These results were double the proportion of anxiety and depression found in those without an IBS diagnosis.
The incidence of anxiety, bipolar disorder, depression, suicidal attempts/ideation, and eating disorders was notably higher in the IBS patient population when compared to the regular adult population.
Most people are able to manage their IBS symptoms by controlling their diet, lifestyle, and stress. While only a small number of people suffering from IBS have severe symptoms, they can be treated with medication in addition to making these other necessary lifestyle and diet modifications.
There are several ingredients found in supplements that offer positive results for overcoming IBS and its symptoms. Adding a quality supplement containing these elements to your daily routine provides your body with additional nutrients and it may also eliminate IBS symptoms.
Although there are no known methods to prevent IBS, there are a few steps you can take that may help keep symptoms at bay:
Medically reviewed by Beverly Timerding, MD.