

Most people think of a fungal infection as a yeast infection or athlete’s foot—they’re itchy and annoying but harmless and relatively easy to treat. However, there are various species of fungi lurking around the world, preying on people with weakened immune systems. Once these fungi enter the human body, they can resist standard antifungal drugs and often cause serious illness or death.
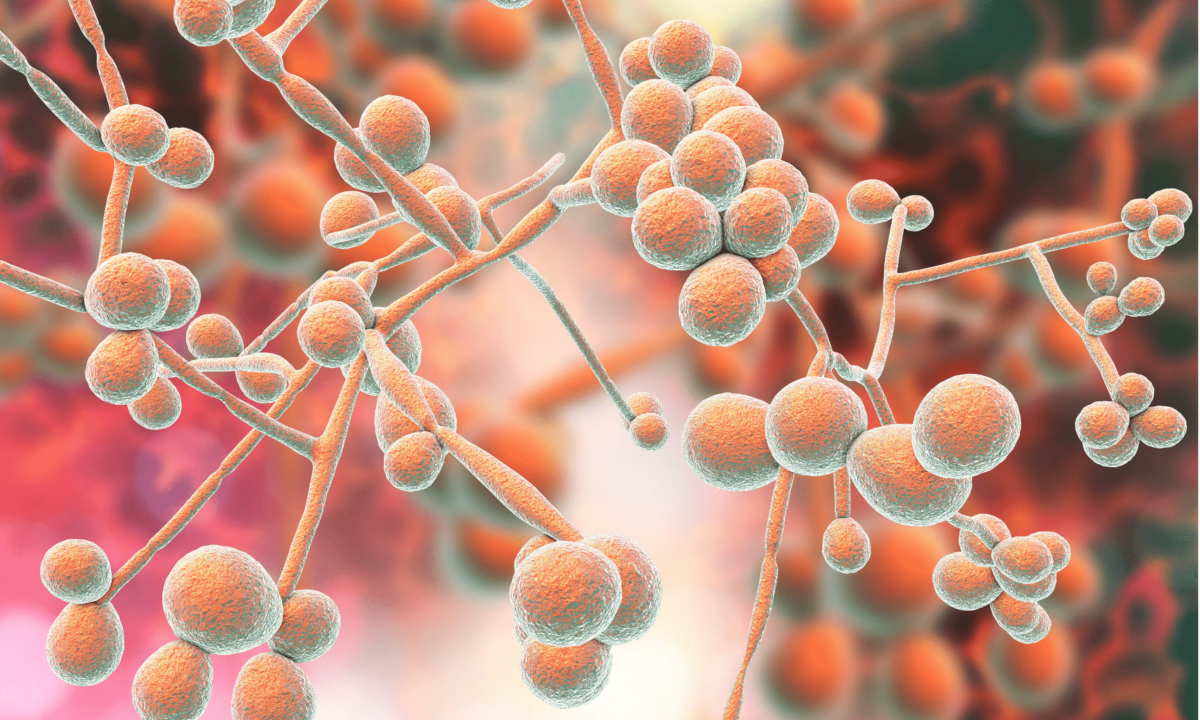
One type of fungus that’s been getting recent media attention, Candida auris, is becoming more prevalent throughout the United States and the world, with a steadily rising death toll. It’s difficult to detect through blood tests because it looks like other, more easily treatable fungal infections. Once identified, treatment can be challenging because of inappropriate management from prior misidentification and the infection’s ability to evade and resist current drug treatments.
The most vulnerable people to these infections are immunocompromised patients like diabetics, those with an organ or tissue transplant, people taking immunosuppressive medications, and anyone receiving chemotherapy. Candida auris is opportunistic, particularly in hospital settings, and can make its way into the body through invasive catheters, ventilators, or surgical treatments.
It’s easily spread from person to person, since it can live on skin with no symptoms, and spreads easily on hospital surfaces (e.g., beds and equipment) when improperly cleaned. A 2018 outbreak in an Oxford University Hospital intensive care unit in the United Kingdom was determined to be caused by multiuse equipment, including axillary thermometers used to measure temperatures under the armpit.
Candida auris and other deadly fungal pathogens like Aspergillus and Pneumocystis are responsible for at least 13 million infections and over 1 million deaths yearly, a fatality rate similar to tuberculosis, HIV, malaria, and breast cancer.
Since deadly fungal infections have risen steadily over the past 50 years, with global death rates similar to some of the worst diseases, why haven’t scientists developed effective treatments to reduce risks for immunocompromised individuals?
The answer involves scientific and economic challenges that must be overcome.
There are hundreds of different antibiotics used to treat bacterial infections, and antivirals have been increasingly effective in fighting off viruses, shortening symptoms, and boosting the immune system. Developing medications to treat fungal infections can be complicated because fungi have the same type of cells as humans, so a substance created to kill fungi may mistakenly target human cells. Many antifungals are highly potent, so if they attack human cells, they can cause kidney or liver damage, particularly after prolonged use [1][2].
Another challenge is the tendency of these fungal infections to become resistant to the few available working medications. There are several reasons why these infections can build resistance to antifungal medications.
The selection of antifungal drugs is limited and becoming less effective because fungi have a sneaky way of evolving to combat current treatments.
Prospective new medicines are in development, but they require additional studies to determine if they are safe and effective.
Immunotherapy has been used for many years to battle cancer successfully by training the immune system to find and destroy cancer cells.
Dr. Zeeshan Afzal, a veterinarian with a background in clinical science and extensive experience with fungal disease, told The Epoch Times, “One example of immunologic therapy for invasive fungal infections is monoclonal antibodies designed to target and neutralize fungal cells specifically.”
Afzal believes another potential approach is to use cytokines, molecules that signal the immune system to respond to these fungal infections. “Research is ongoing, and there have been some promising findings in this area.”
There are more than 25 vaccines available worldwide, but none can protect vulnerable, immunocompromised patients from fungal infections.
Karen Norris, who holds a doctorate in biomedical sciences and microbiology, a member of the University of Georgia Center for Vaccines and Immunology, is working to find a vaccine to protect against the fungal pathogens responsible for more than 80 percent of fatal fungal infections.
Researchers tested the efficacy in four preclinical animal trials. They relied on different immunosuppressed models to reflect drug regimens similar to at-risk human patients like transplant recipients or cancer patients. The vaccine effectively produced protective antibodies in each model.
“Because it targets three different pathogens, the vaccine has the potential to be groundbreaking regarding invasive fungal infections,” Norris told UGA Today. Plans are underway to develop the vaccine for a Phase 1 (human) safety trial.
While research continues, a vaccine will not be available anytime soon since human trials will likely continue through the next five years.
Fungal infections cost the health care system millions of dollars each year. According to the journal Open Forum Infectious Diseases, in 2018, there were 666,235 fungal infections diagnosed in the United States. The estimated hospitalization costs directly associated were $6.7 billion in one year, with a total cost of $37.7 billion for all visits where any fungal infections were diagnosed. Ultimately, the fungal infections doubled the cost to the patient, the hospital stay, and the risk of death in patients considered at-risk.
Yet there is little talk among the media or government officials about the urgency to solve this overwhelming problem in the United States and worldwide.
The most likely reason is that these costly and deadly fungal infections primarily target patients with compromised immunity. The death rate for this at-risk population is estimated at over a million yearly, but pharmaceutical companies may not have a financial incentive to fund research and development for efficacious drugs, therapies, or vaccines [3].
While the development of effective fungal treatments may reduce the cost of medical care, which is already nearly unsustainable in the United States, pharma companies are looking to profit. Dennis Dixon, who leads bacterial and fungal research at the National Institutes of Health, told Vox on March 24, “It’s going to take someone to develop that tough market for this to go forward.”
Invasive and often deadly fungal infections continue to plague the immunocompromised across the globe. The science exists to develop better antifungal drugs, immunologic therapies, and effective vaccines. Possibly the most compelling reason for the private sector to increase funding for life-saving therapies would be the millions of lives they could save.
