Although vaccines have been glorified as the best strategy in dealing with infectious diseases, limited understanding of the wisdom of the immune system is what’s pushing that conclusion. Our bodies are able to separate the wheat from the chaff when it comes to invading pathogens, or when a vaccine stimulates the attack.
A study (pdf) published in Science Immunology in 2022 showed incrementing doses of the mRNA boosters prompted a change in our immune systems. The immune system then gains a false sense of security without the need to make a strong counterattack against the vaccine, as the vaccine is not the real virus. Worse, the boosters might not even induce any effect in one category of people whose members are at high risk of severe infection.
According to the study, the third dose of the mRNA vaccines seems to be linked with a class switch in subtypes of immunoglobulin G (IgG), the dominating serum antibody in our immune system, which raises the question of immune exhaustion. Class switching is when B cells redirect their efforts toward producing IgG. To start, they produce generic immunoglobulin cells like IgM. But once they find that the invading pathogen is tougher than they thought, they switch to producing the more effective IgG to ward off the infection.
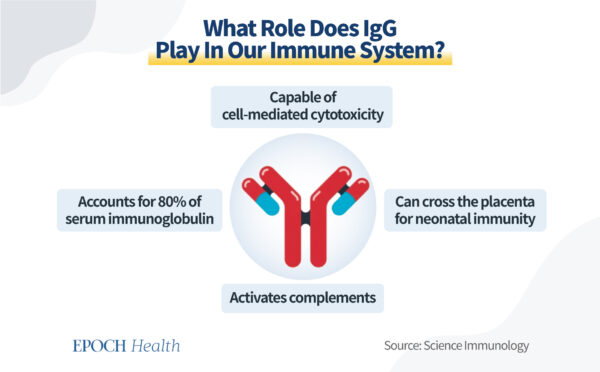
IgG is an important serum antibody that makes up roughly 80 percent of all antibodies in our immune system. After class switching occurs, B cells release different types of IgG instead of other less effective immunoglobulin cells. Depending on the severity of the infection, the ratio of IgG may also vary.
IgG is the more effective fighter in our immune system, as it has the ability to opsonize and fixate complements, meaning that it attaches to infected cells or pathogens and instructs killer cells to swallow intruders up through phagocytosis. It is also the only antibody that crosses into the placenta, playing a critical role in protecting the unborn fetus.
However, IgG is split up into four major subtypes—denoted IgG1 through IgG4—and each has its own strengths and limitations.
Out of all four, IgG1 makes up most of serum IgG as it has the best immune properties. Along with IgG3, these two are the most potent members of the IgG family.
IgG4 is considered one of the weakest types, as it doesn’t do as well in attracting immune cells responsible for eliminating invaders.
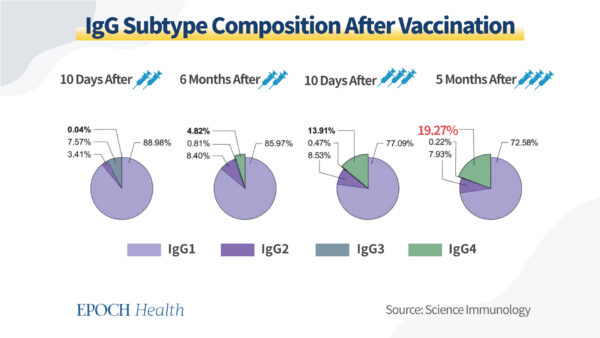
Research shows that IgG4 composition usually hovers around 4 percent, a number matched by the aforementioned study for patients after five months of receiving the second dose of vaccine.
Right after the second dose, IgG4 levels were at 0.04 percent while IgG1 and IgG3–the most potent members in the IgG family–made up 96.55 percent of all IgG, according to the aforementioned Science Immunology paper.
This change in IgG levels indicates that the body interprets the second dose as a serious infection and produces the more effective IgG to tackle the simulated infection. However, things look a little different after the booster shot.
In the study, the percentage of IgG4 in the blood serum rose to unexpectedly high levels after the third dose. Ten days after the third vaccination, IgG4 levels rose to 13.91 percent and jumped to 19.27 percent five months after. At the same time, IgG1 and IgG3 levels both dropped, showing a significant change in blood serum antibody composition.
This is not good, as higher levels of IgG4, without the ability to stimulate immune cells, could indicate immune exhaustion. It is also an indication that the immune system intentionally dampened the response starting with the third dose of the vaccination.
On the other hand, although IgG3 and IgG1 contribute the most to immune mechanisms, the downside is that they are costly to produce and can quickly wear out the body. In contrast, IgG4 isn’t as effective yet more economical to produce.
The immune system will always place warding off outside intruders at the top of its to-do list while keeping efficiency in mind. This is why the amount of each IgG subtype produced varies with each infection.
In the Science Immunology study, high IgG4 levels after the third dose, even a long time after it, indicate that the immune system is being worn out through the repeated vaccination course. The body treats the third dose with more indifference and deploys the less effective IgG4 in response.
This development of more IgG4 than usual is unhealthy and riskier for people if they encounter the real virus later, as COVID-19 can develop into a rather severe disease, especially for people with chronic conditions. If the body begins to treat the SARS-CoV-2 vaccine like a boy crying wolf, then what if the real virus comes knocking at the door?
The vaccine is meant to train the immune system’s memory cells so that the next time something similar comes along, they know how to quickly defend the immune system. This process is also called antibody acquisition. The aforementioned study demonstrates that the body stops regarding COVID-19 as a serious viral infection after the booster shot. However, in some people, the boosters actually have no effect at all.
One group of people that might gain the least from vaccination seems to include those who are immunocompromised, like organ transplant recipients—people who regularly take immunosuppressants as a part of post-operational procedures.
A study published in Nature showed that antibody acquisition rates against COVID-19 were “extremely low” in kidney transplant patients. This finding contradicts the purpose of the vaccine, as the vaccine is meant to induce antibody acquisition.
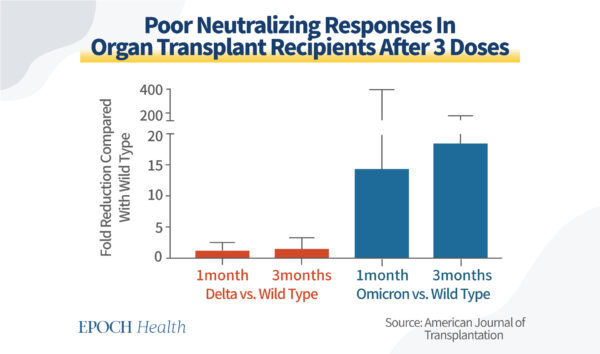
Similar reports have also surfaced elsewhere, especially in regard to newer variants of COVID-19. An observational study claiming to be the largest when analyzing four-dose vaccinated organ transplant recipients shows that the mRNA vaccine booster demonstrates a “lack of formal neutralization” against “variants of concern including Omicron.”
Data (pdf) also show that antibody neutralization against Omicron has seen a 15–20-fold reduction when compared with the wild-type virus in transplant recipients. These findings are of grave concern.
The U.S. Centers for Disease Control and Prevention still recommends immunocompromised people receive a COVID-19 vaccine as well as get their boosters.
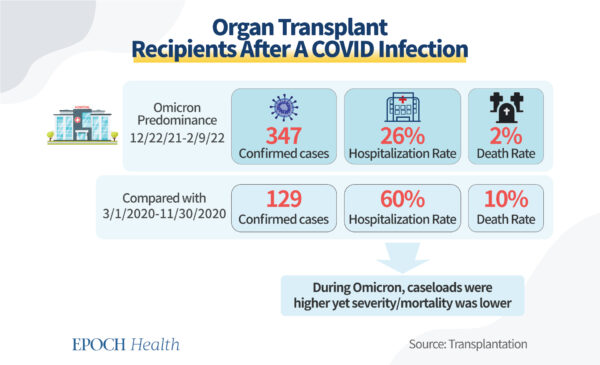
According to data published in the medical journal Transplantation, during the recent Omicron wave, although COVID-19 cases have increased for organ transplant recipients, the death rate of this population dropped fivefold.
However, is this reduction due to repeated vaccination or to the reduced pathogenicity of Omicron variants? Is it really effective to drive vaccination campaigns for the immunocompromised, based on the trifling level of antibody acquisition? Can the benefits of repetitive boosting outweigh the increased risk of side effects?
It is really time to reconsider what place the COVID-19 vaccines should take. Are we underestimating the wisdom of our immune system? This stance is similar to that taken in a previous article that mentioned how “negative efficacy” should have stopped vaccine recommendations in their tracks.
Now researchers are saying that vaccines, especially boosters, fail to have a significant effect on the immunocompromised—the very group of people especially susceptible to severe disease and death. We need to stop placing the mRNA shots on a pedestal and consider all options in response to SARS-CoV-2, such as focusing on bolstering our natural immune system and holistic well-being.
Views expressed in this article are the opinions of the author and do not necessarily reflect the views of The Epoch Times. Epoch Health welcomes professional discussion and friendly debate. To submit an opinion piece, please follow these guidelines and submit through our form here.